Does Targeting BMI Help Reduce Racial Disparities and Improve Outcomes in Stage III Colorectal Cancer Patients?: A Retrospective Study
Prajwal Boddu, Mebea Aklilu and Dana Villines
Prajwal Boddu1*, Mebea Aklilu2 and Dana Villines3
1Department of Internal Medicine, Advocate Illinois Masonic Medical Center, Chicago, IL, USA
2Department of Hematology/Oncology, Advocate Illinois Masonic Medical Center, Chicago, IL, USA
3 Department of Research, Advocate Healthcare, Advocate Illinois Masonic Medical Center, Chicago, IL, USA
- Corresponding Author:
- Prajwal Boddu
Department of Internal Medicine, Advocate Illinois Masonic Medical Center, 856 West Nelson Street, Apt 2002, Chicago, IL 60657, United States of America.
Tel: 4087727340
E-mail: bprajwalc@gmail.com
Received date: May 23, 2016; Accepted date: June 10, 2016; Published date: June 16, 2016
Citation: Boddu P, Aklilu M, Villines D. Does Targeting BMI Help Reduce Racial Disparities and Improve Outcomes in Stage III Colorectal Cancer Patients?: A Retrospective Study. Colorec Cancer 2016, 2:2.
Abstract
Objective: In this study, we determined the association of BMI with stage 3 colorectal cancer (CRC) outcomes by ethnicity. We tested the hypothesis that obesity is associated with worsening CRC survival in the minority ethnicity groups. The study was intended to evaluate the role of BMI in the minority groups in accounting for these differing outcomes, in which case, results from this study may influence preventive risk strategies in the high risk ethnicity groups by targeting modifiable risk factors such as high BMI.
Methods: We utilized the cancer registry database and included the following data: age, sex, ethnicity, chemotherapy regimen, BMI. Outcome variables of recurrence time and overall survival were censored at 10 years and survival curves with Kaplan-Meier estimates were used to compare recurrence and survival between various BMI categories in the major racial/ ethnic study groups. Cox regression models were used to determine if BMI is a predictor of CRC recurrence and survival for each ethnicity group.
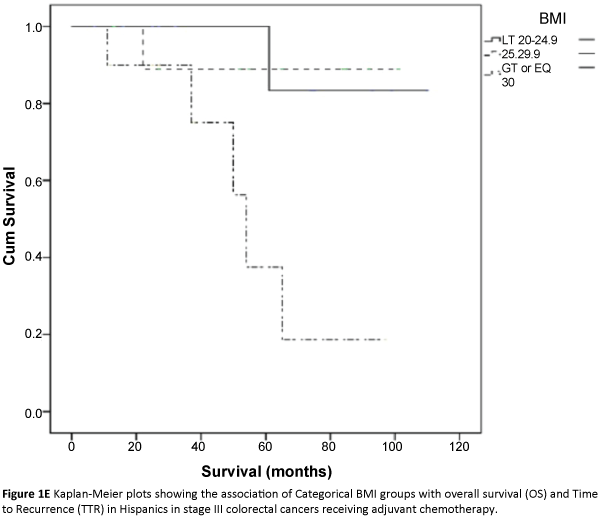
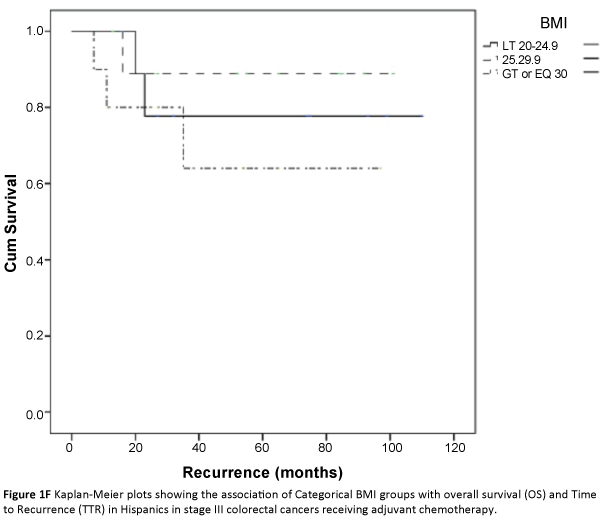
Results: Across the BMI categories, we did not find any significant association between categorical BMI and TTR (HR 2.1(0.76-5.83), p=0.15), (HR 0.91(0.68- 1.21), p=0.52), (HR 1.13(0.43-2.86), p=0.83) or overall survival (HR 1.39(0.6-3.1), p=0.41), (HR 0.88(0.65-1.20), p=0.43), (HR 3.7(0.14-12.48), p=0.49) in African Americans, Caucasians and Hispanics respectively.
Conclusions: Overweight and obese patients were not associated with increased risk of recurrence or decreased overall survival in either of the three major ethnic study groups. Targeting BMI as potential risk strategy, may not affect the final outcomes in stage III colorectal cancer irrespective of underlying ethnicity. However, it is important to encourage a healthy lifestyle and promote weight reduction. The prevalence of obesity and its impact on survival outcomes needs to be studied in the lower stage groups and younger aged minority populations to help inform preventive risk strategies and potentially reduce existing racial disparities.
Keywords
BMI; Colorectal cancer; Stage III; Race; Ethnicity; Overall survival; Recurrence
Introduction
Obesity is an established modifiable risk factor associated with increased incidence of advanced colorectal cancer (CRC) [1]. BMI, an approximation of general adiposity, has traditionally been used as a marker for obesity in clinical epidemiological studies. Results from studies addressing the prognostic impact of high BMI at the time of diagnosis on colorectal cancer outcomes have, thus far, been conflicting and inconsistent. A prospective observational study by Mayerhard et al. showed that there was no significant association between BMI and CRC outcomes [2], while other studies have reported statistically significant worse outcomes in underweight and obese CRC survivors [3-6]. A Recent metaanalysis reported the BMI pre and post-diagnosis is associated with increased risk of colorectal cancer related mortality and all-cause mortality [7]. Studies suggest that the strength of association between BMI and colorectal cancer survival varies by factors such as distribution of adiposity, demographic variables such as age and sex, and methodological variables as in the type of measure of obesity used in the study design [3,7,8]. The association of BMI with CRC survival by race/ethnicity has not been studied to date.
Ethnic/racial differences in the incidence of cancer has been well documented in epidemiological studies with notably worse outcomes in the ethnic minority groups [9,10]. Ethnic groups also vary in the prevalence of obesity. Socioeconomic factors resulting in lack of access to health care and unequal health utilization contribute to this racial disparity. However, studies have shown cancer disparities in survival to exist even after adjusting for these complex socioeconomic variables. This disparity is more pronounced in the younger age group Hispanics and African Americans, a population not covered by the current screening guidelines [11-13]. Biological factors relating to ethnic genetic differences, tumor biology and location have also been shown to play an important role [11-15]. Alternatively, potentially modifiable risk factors such as higher prevalence of obesity and decreased physical activity have been posited as contributing factors to the higher incidence in these groups but not been studied in great detail.
Methods
This was a retrospective chart review on patients with a diagnosis of TNM stage III Colorectal cancer from 2005 to 2015. Data was collected from the Advocate Cancer Center registry, involving three Advocate Hospitals in Chicago. Institutional Review Board approval was obtained prior to study conduct. Patients were excluded from the study if they did not receive adjuvant chemotherapy for any reason. 354 consecutive patients were deemed eligible for the study. We abstracted the following data for analysis: age, gender, ethnicity/race, chemotherapy regimen, hospital/geographic area, tumor location (proximal vs distal), BMI/height and weights at the time of diagnosis to assess for clinical cancer outcomes. Socioeconomic factors were not considered for analysis, given that patients had equal access to health care and there were no problems with medication assistance or insurance coverage.
BMI was classified as per WHO classifications into: underweight, BMI <20 kg/m2; normal-weight, 20 to 24.9 kg/m2; overweight, 25 to 29.9 kg/m2; class 1 obesity 30-34.9 kg/m2, class 2 obesity >35 kg.m2 [16]. Ethnic categories: Hispanics included all patients of Cuban, Mexican, Puerto Rican, South or Central American or other Spanish culture or origin. Asian/Indian included patients of Indian, Chinese, Korean, Japanese and south Asian origin. Other ethnicities constituted very few numbers and were classified as other, which included Native Americans, multiracial Americans, native Hawaiians, Pacific Islanders, Middle Easteners including Tumor location was classified into 1) proximal, which included tumors of cecum, ascending colon, hepatic flexure, transverse colon, splenic flexure and 2) distal which included tumors of descending colon, sigmoid, recto sigmoid, rectal location. Data was not available on the methodology of surgical approach.
Chemotherapy regimen was categorized into two groups: based on whether they received: A) 5-FU (5-FU+Avastin; 5-FU; Capacetabine; 5-FU+Avastin) or B) 5-FU+oxaliplatin (FOLFOX 4; FOLFOX 6; FOLFOX+Avastin; Capectabine+Ox). Patients receiving bevacizumab were not included in a separate category.
Statistical analysis
Descriptive statistics were presented as means and standard deviations for continuous data and as counts and percentages for dichotomous and categorical data. Time to recurrence (TTR) was determined as the time in months from the initial diagnosis to determination of local or distant recurrence. Overall survival (OS) was determined as duration in months from the time of initial diagnosis to death as final outcome. Outcome variables were censored at 10 years and survival curves with Kaplan- Meier estimates were used to compare recurrence and survival between various BMI categories in each major racial/ ethnic study group. Cox regression models were used to determine if BMI is a predictor of CRC recurrence and survival for each ethnicity group. Analysis was performed using SPSS®21 (Chicago, IL, USA) and statistical significance was determined at p=0.05.
Results
The study included 354 patients with TNM stage 3 colorectal cancer patients who participated in 5-FU or FOLFOX adjuvant chemotherapy. The percentage of patients from the three cancer centers were 37%, 43%, and 20% respectively. Caucasians represented the largest ethnicity group constituting 68% of the study population (Table 1). African American, Hispanics, and Asians represented 13.6%, 8.8%, 5.1% of study population respectively (Table 1). BMI was measured at the time of diagnosis and categorized per current WHO classification [16]. In this cohort of patients, 37.6% were overweight and 33.6% were obese (Table 1). The median BMI was 25.4. After a median follow-up of 10 years, 24.3% (N=86) of patients had cancer recurrence and 21.5(N=76) had died (Table 1). The mean time to recurrence was 91.6 months and mean time of OS was 93.3 months (Table 1). After analyzing data, we noted very few patients belonging to minor ethnic groups and represented a highly heterogenous category. Hence, we did not proceed with further analysis of these subsets. Median ages of the African American, Hispanic and Caucasian study patients were 61.5, 66, and 69 respectively. 65% of African Americans’ and 63% of Hispanics’ tumors were proximal in location. Patients receiving combination chemotherapy had improved survival outcomes compared to patients receiving monotherapy, but this did not reach statistical significance (95.2 ± 3.4 vs 81.9 ± 6; p=0.07). There was no difference in time to recurrence (p=0.34).
| Total sample (n=354) | |
|---|---|
| Age (mean) | 63 |
| BMI (median) | 25.4 |
| Underweight (%) | 13(3.7%) |
| Normal (%) | 89(25.1%) |
| Overweight (%) | 133(37.6%) |
| Obesity class I (%) | 57(16.1%) |
| Obesity Class II and above (%) | 62(17.5%) |
| Gender | |
| Male (%) | 182(51.4%) |
| Race | |
| African American (%) | 48(13.6%) |
| Asian/Indian (%) | 18(5.1%) |
| Hispanic (%) | 31(8.8%) |
| Caucasian (%) | 241(68.1%) |
| Other (%) | 16(4.6%) |
| Stage | |
| 3A | 51(14.4%) |
| 3B | 210(59.3%) |
| 3C | 93(26.3%) |
| Chemotherapy | |
| Group A | 223(63%) |
| Group B | 72(20.3%) |
| Tumor location | |
| Proximal (%) | 178(52.7%) |
| Outcomes | |
| Number of recurrences (%) | 86(24.3%) |
| Number of deaths (%) | 76(21.3%) |
Table 1: Baseline characteristics of patient population.
Across the three treatment centers, we found no statistically significant difference in the rate of tumor recurrence or overall survival. Also, there was no association noted between race/ ethnicity and colorectal cancer survival outcomes (TTR 1.01 (0.80-1.28); OS 0.90(0.75-1.15)).
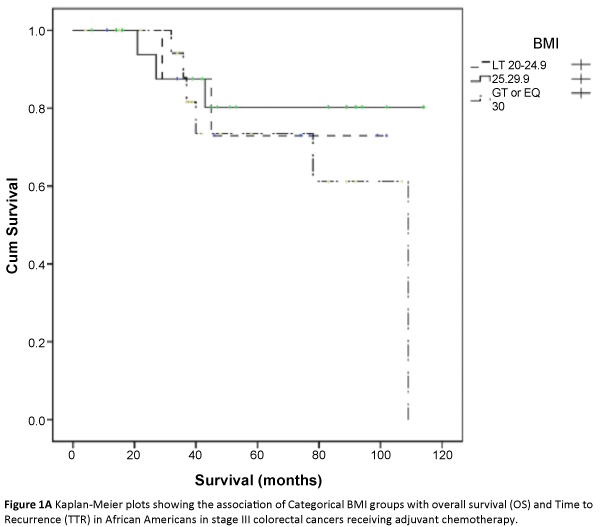
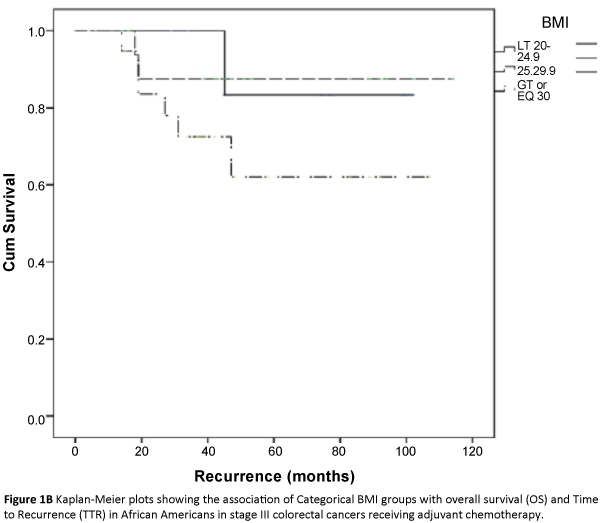
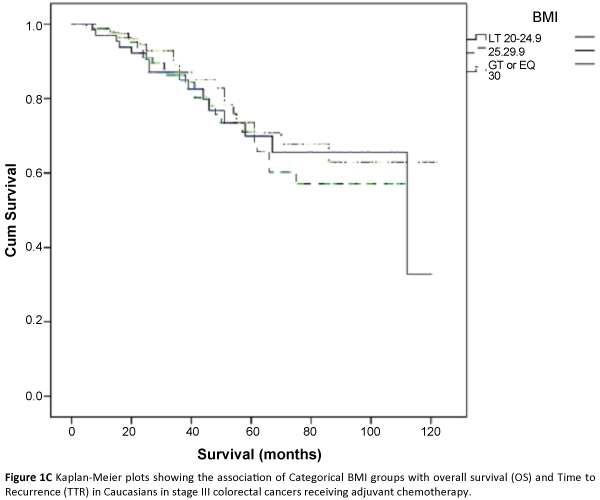
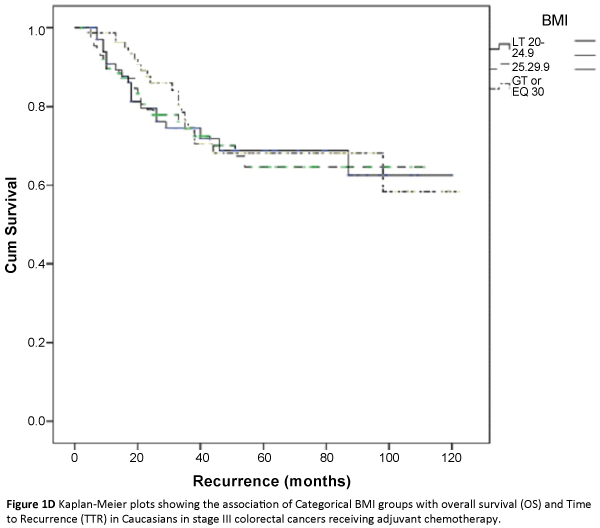
The three major ethnicity populations in our study included Caucasians, Hispanics and African Americans. The Asian/Indians and various minority groups (classified under ‘other’) constituted a very small proportion and were not included in further analysis due to small sample size estimates. In a univariate analysis, we analyzed the association of categorical BMI with overall survival and time to recurrence outcomes in each of the three major ethnicity study populations i.e., African Americans, Caucasians and Hispanics after adjusting for covariates. Across the BMI categories, we did not find any significant association between categorical BMI and TTR [(HR 2.1(0.76-5.83), p=0.15), (HR 0.91(0.68-1.21), p=0.52), (HR 1.13(0.43-2.86), p=0.83)] or overall survival (HR (1.39(0.6-3.1), p=0.41), (HR 0.88(0.65-1.20), p=0.43), (HR 3.70(0.14-12.48), p=0.49)] in African Americans, Caucasians and Hispanics respectively (Table 2; Figures 1A-1F). Overweight and obese patients were not associated with increased risk of recurrence or decreased overall survival in either of the three major ethnicity study groups.
| Time of Recurrence | Overall Survival | |||
|---|---|---|---|---|
| Categorical BMI | HR*(95%CI) | P-Value | HR*(95% CI) | P-Value |
| African Americans | 2.1[0.76-5.83] | 0.15 | 1.39[0.60-3.1] | 0.41 |
| Caucasians | 0.91[0.68-1.21] | 0.52 | 0.88[0.65-1.20] | 0.43 |
| Hispanics | 1.13[0.43-2.86] | 0.83 | 3.70[0.14-12.48] | 0.49 |
*- adjusted for age, gender, hospital/geographic area, tumor location, type of chemotherapy.
Table 2: Association between Categorical BMI and Colorectal cancer outcomes.
Discussion
Based on our study, there was no statistical association between categorical BMI and cancer recurrence and mortality in TNM Stage 3 CRC patients. Also, our study did not find any statistical association between categorical BMI and colorectal cancer outcomes in either major ethnicity study group i.e., African Americans, Caucasians and Hispanics. This argues to the fact that even though there might exist a higher prevalence of obesity in the minority groups (i.e., Hispanics and African Americans), it may not have a role to play in explaining worsening outcomes in these ethnicity groups. However, it is important to note that our study population was confined to stage III CRC patients. Very few studies have looked at the interaction of BMI and race in colorectal cancer outcomes. A study by Min et al. demonstrated a favourable overall survival in Asian CRC patients who had a BMI compared to normal weighted individuals (BMI>23). There is no data available on the role of categorical BMI in other ethnicity groups. Our study results have important implications in that, although BMI is a modifiable risk factor, targeting it as potential risk strategy, may not affect the final outcomes in stage III colorectal cancer irrespective of underlying ethnicity. An important caveat to this interpretation is that weight change and its potential role was not analyzed and warrants further study.
Ethnic/racial differences in the incidence and prognosis of cancer has been documented in epidemiological studies with worse outcomes in the ethnic minority groups (Table 3). Socioeconomic factors resulting in lack of access to health care and unequal health utilization contribute to this racial disparity [17]. However, studies have shown cancer survival disparities to exist even after adjusting for complex socioeconomic variables. This disparity is more pronounced in the younger age group Hispanics and African Americans [11-13]. The influence of race on CRC outcomes has been well studied comparing African Americans and Caucasian populations. African American (AA) population has inferior survival outcomes when compared to Caucasian whites and present with higher stages at time of diagnosis. However, even controlling for stage, socio-demologic factors, performance status, and tumor characteristics, lower nutritional status does not completely explain the disparity in black population [18-20]. Similarly, other studies have demonstrated inferior CRC cancer survival rates in Hispanic whites when compared to their Caucasian counterparts. Blacks and Hispanics are significantly more likely to develop advanced distal stage III and IV colorectal cancers than proximal cancers; location of the tumor with its associated biological characteristics may account, to an extent, in explaining the higher mortality risk in these two ethnic groups compared to Caucasians [21-26]. Secondly, racial disparity seems to be confined to earlier stages, with similar survival outcomes in higher stage (stage IV) AA and Caucasian population [20]. The racial disparities seem diminish with advancement in stage of CRC and age at diagnosis [12,20,21] (Table 3). We did not find a statistical association between ethnicity and colorectal cancer outcomes. In our study, 65% of African Americans’ and 63% of Hispanics’ tumors were proximal in location, as is expected in a higher age population. Advanced stage (TNM Stage 3) and the high proportion of proximal tumors in the minority age groups of our study population account for the lack of racial disparity in CRC outcomes. It has been shown that the existing disparity is more pronounced in the younger age group Hispanics and African Americans, a population not covered by the current screening guidelines. Our study cohort involved AA, Hispanics and Caucasians with similar median age of 61.5, 66, and 69 respectively, a much older age group where race specific aggressive tumor biology characteristics are not expected to play a major role in creating survival outcome disparities. Prevalence of obesity and the association between categorical BMI and survival outcomes in the lower cancer stages (I and II) needs to be studied as it is in these groups that the racial disparities have been shown to be the highest.
| Reference study number |
Study type | Study period |
Total Patient cohort(n) |
Stages involved |
Ethnicity comparison of interest |
RR(95% CI) | Adjustment factors |
|---|---|---|---|---|---|---|---|
| 17 | Retrospective cohort |
1984-1997 | 617 | I-IV | African americans(AA), Caucasians(C) |
AA vs C on OS: 1.5(1.2-1.9) |
Gender, site, socioeconomic factors, Therapeutic modalities |
| 14 | Retrospective cohort |
1988-2007 | 975 | I-IV | Africans Americans, Caucasians, Hispanics(H) |
AA vs C on OS: 1.2(1.16-1.24) H vs C: 1.07(1.03-1.12) |
Age, sex, primary tumor site, income, education, residence, stage, use of adjuvant therapy |
| 20 | Prospective observational | 1986-1990 | 2,713,474 | I-IV | African Americans, Caucasians |
AA vs C on OS: All stages: 1.2(1.0-1.5) Stage 2: 1.8(1.0-3.1) Stage 3: 1.5(1.0-2.3) Stage 4: not significant |
Age, sex, geographic area, stage |
| 21 | Retrospective cohort |
1988-2000 | 154,103 | I-IV | African Americans, Caucasians, Hispanics |
AA vs C on OS: All stages: 1.2(1.2-1.3) Stage I/II: 1.4(1.3-1.5) Stage III/IV: 1.1(1.1-1.2) H vs C on OS: All stages 1.1(1.1-1.2) Stage I/II: 1.4(1.2-1.5) Stage III/IV: 1.0(1.1-1.2) |
Age, year, SEER registry, surgical and radiation treatment, stage |
| 25 | Retrospective cohort | 1989-1994 | 3186 | I-IV | African Americans, Caucasians |
AA vs C on OS: | Demographics, comorbidity, metastasis, tumor location |
| Current study | Retrospective cohort | 2005-2015 | 354 | III | African Americans, Caucasians, Hispanics |
Age, gender, BMI, hospital/geographic area, type of chemotherapy |
Table 3: Cohort studies of race/ethnicity on survival outcomes in colorectal cancer patients.
Few limitations of our study must be considered. Race/ethnicity was determined based on medical chart reviews and it is possible that there was a certain degree of misclassification. Also, we categorized the patients into very broad ethnic categories of Asian/Indian and Hispanic which umbrella highly heterogeneous subgroups and were able to study only the three major ethnicity groups due to limited population size. Other limitations of our study include retrospective study design and relatively small sample size with limited power to detect statistically significant outcomes. We used BMI as the only adiposity marker to assess outcomes in our study. BMI is a marker of overall obesity whereas other measures like Waist circumference (WC) and waist-to-hip (WHP) ratio account better for central obesity. In some studies, WHR and WC were more predictive of the risk of developing colon cancer than BMI [27]. Strengths of the study include the fact that BMI was measured by trained staff and not by selfreported questionnaires.
Conclusions and Future Study
In conclusion, categorical BMI is not statistically associated with colorectal cancer outcomes in African Americans, Caucasians or Hispanics. Targeting BMI as potential risk strategy may not influence the final outcomes in stage III colorectal cancer irrespective of underlying ethnicity. It is important to encourage a healthy lifestyle and promote weight reduction irrespective of ethnicity. Our study was confined to the older aged stage 3 CRC patients. The prevalence of obesity and its association with colorectal cancer outcomes in lower stage CRC and younger aged high-risk minority ethnicity populations needs further study to help inform preventive risk strategies and potentially reduce existing racial disparities.
References
- Stein B, Anderson JC, Rajapakse R (2010) Body mass index as a predictor of colorectal neoplasia in ethnically diverse screening population.Dig Dis Sci 55:2945-2952.
- Meyerhardt JA, Niedzwiecki D, Hollis D(2008) Impact of body mass index and weight changeafter treatment on cancerrecurrence and survival in patients with stage III colon cancer: findings from Cancer and Leukemia Group B 89803. J ClinOncol26:4109-4115.
- Sinicrope FA, Foster NR, Yothers G (2013) Body mass index at diagnosis and survival among colon cancer patients enrolled in clinical trials of adjuvant chemotherapy. Cancer 119:1528-1536.
- Dignam JJ, Polite BN, Yothers G (2006) Body mass index and outcomes in patients who receive adjuvant chemotherapy for colon cancer. J Natl Cancer Inst98:1647-1654.
- Campbell PT, Newton CC, Dehal AN, Jacobs EJ, Patel AV, et al. (2012) Impact of body mass index on survival after colorectal cancer diagnosis: the Cancer Prevention Study-II Nutrition Cohort.J ClinOncol30:42-52.
- Sinicrope FA, Foster NR, Sargent DJ (2010) Obesity is an independent prognostic variable in colon cancer survivors. Clin Cancer Res16:1884-1893.
- Lee J, Meyerharst JA, Giovannucci E, Jeon JY (2015) Association between Body Mass Index and Prognosis of Colorectal Cancer: A Meta-Analysis of Prospective Cohort Studies10: e0120706.
- Thompson CL, Berger NA, Chak A, Li L (2012) Racial differences in measures of obesity and risk of colon adenoma. Obesity (Silver Spring) 20:673-677.
- Jinjuvadia R, Jinjuvadia K, Liangpunsakul S (2013) Racial disparities in gastrointestinal cancers-related mortality in the U.S. population. Dig Dis Sci58:236-243.
- Ward E, Jemal A (2004) Cancer disparities by race/ethnicity and socioeconomic status.CA Cancer J Clin54:78-93.
- Cruz-Correa (2013 Increasing colorectal cancer burden among young US Hispanics: is it time to change current screening guidelines?Dig Dis Sci58:1816-1818.
- Stefanidis D, Pollock BH, Miranda J (2006) Colorectal cancer in Hispanics: a population at risk for earlier onset, advanced disease, and decreased survival. Am J ClinOncol29:123-126.
- Xicola R, Gagnon M, Clark JR (2014) Excess of proximal microsatellite-stable colorectal cancer in African Americans from a multi-ethnic study.Clin Cancer Res 20: 4962-4970.
- Aizer AA, Wilhite TJ, Chen MH (2014) Lack of reduction in racial disparities in cancer-specific mortality over a 20-year period.Cancer120:1532-1539.
- Laiyemo AO, Doubeni C, Pinsky PF (2010) Race and colorectal cancer disparities: health-care utilization vs different cancer susceptibilities.J Natl Cancer Inst102:538-546.
- The World Health Report 2000 - Health systems: improving performance(2001) Public Health Rep 116: 268–269.
- Govindarajan R, Shah RV, Erkman LG, Hutchins LF (2003) Racial differences in the outcome of patients with colorectal carcinoma. Cancer 97:493-498.
- McCutchen AS, Munoz JC, Brenner L, Wludyka P, Vega KJ (2011) Lower albumin levels in African Americans at colon cancer diagnosis: a potential explanation for outcome disparities between groups? Int J Colorectal Dis 26:469-472.
- Chen VW, Fenoglio-Preiser CM, Wu XC, Coates RJ, Reynolds P, etal. (1997) Aggressiveness of colon carcinoma in blacks and whites. National Cancer Institute Black/White Cancer Survival Study Group. Cancer Epidemiol Biomarkers Prev6:1087-1093.
- Mayberry RM, Coates RJ, Hill HA, Click LA, Chen VW, et al. (1995) Determinants of black/white differences in colon cancer survival. J Natl Cancer Inst 87:1686-1693.
- Chloe CMS, Libby MM, Jamie TBSN,Christopher IL (2005) Differences in colorectal carcinoma stage and survival by race and ethnicity. Cancer 104: 629–639.
- Min YW, Kim SA, Lee JH, Kim JY, Chang DK, etal. (2012) Overweight is associated with a favorable survival in patients with colorectal cancer: a prospective cohort study in an Asian population. SurgOncol 19: 3460-3464.
- Wudel LJ, Chapman WC, Shyr Y, Davidson M, Jeyakumar A, et al. (2002) Disparate outcomes in patients with colorectal cancer: effect of race on long-term survival. Arch Surg 137: 550-556.
- Loupakis F, Yang D, Yau L, Feng S, Cremolini C, et al. (2015) Primary tumor location as a prognostic factor in metastatic colorectal cancer. J Natl Cancer Inst24: 107.
- Dominitz JA, Samsa GP, Landsman P, Provenzale D (1998) Race, treatment, and survival among colorectal carcinoma patients in an equal-access medical system. Cancer 82:2312-2320.
- Pappas AV, Lagoudianakis EE, Dallianoudis IG, Kotzadimitriou KT, Koronakis NE, etal. (2010) Differences in colorectal cancer patterns between right and left sided colorectal cancer lesions. J BUON 15:509-513.
- Moore LL, Bradlee ML, Singer MR, Splansky GL, Proctor MH, et al. (2004) BMI and waist circumference as predictors of lifetime colon cancer risk in Framingham Study adults.Int J ObesRelatMetabDisord 28:559-567.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences