Malignant Small Bowel Tumor - Case Series and Literature Review
Alves Junior AJT*, Romero Machuca ME, Ribeiro RG, Garisto AM, de Oliveira LH, Banci SO, Simoes Neto J, Kagohara OH, Reis Junior JA and Reis Neto JA
DOI10.21767/2471-9943.100034
Alves Junior AJT*, Romero Machuca ME, Ribeiro RG, Garisto AM, de Oliveira LH, Banci SO, Simoes Neto J, Kagohara OH, Reis Junior JA and Reis Neto JA
Clinica Reis Neto, R Gen Osorio, 2273-Cambui, Campinas, SP, Brazil
- Corresponding Author:
- Antonio Jose Tiburcio Alves Junior
Clinica Reis Neto, R Gen Osorio, 2273-Cambui, Campinas, SP, Brazil.
Tel: 551932355611
E-mail: antonio_xxxv@yahoo.com.br
Received: February 21, 2018; Accepted: February 26, 2017; Published: March 03, 2018
Citation: Alves Junior AJT, Romero Machuca ME, Ribeiro RG, Garisto AM, de Oliveira LH, et al. (2018) Malignant Small Bowel Tumor - Case Series and Literature Review. Colorec Cancer Vol.4 No.1:1.
Abstract
Introduction: The diagnosis of malignant small bowel tumors is difficult due to the rarity of these lesions and the lack of presenting signs and symptoms. This fact may delay the treatment and therefore worsen the outcome.
Material and methods: This article describes 6 cases of this rare disease, reviewing the literature on its clinic, pathological and treatment aspects.
Discussion: Malignancies involving the small intestine are rare and account for less than 3% of the gastrointestinal tract cancers. When the different regions of the intestine are considered, adenocarcinomas are mostly found in the duodenum while stromal tumors are usually spread throughout the entire small bowel. Adenocarcinoma represents 33% of MSBT and is best managed with wide segmental surgical resection and primary and regional node lymphadenectomy. Sarcomas represent 17% of MSBT and are treated with en bloc segmental resection with tumor-free margins, with preservation of the tumor’s pseudocapsule. Secondary neoplastic involvement of the small intestine is more common than primary small neoplasia and its treatment is palliative.
Conclusion: MSBT have a rare incidence, however attention and investigation of persistent symptoms may lead to an early diagnosis and treatment.
Keywords
Malignant small bowel tumors; Carcinoid; Adenocarcinoma; Stromal tumors; Melanoma
Introduction
The diagnosis of malignant small bowel tumors (MSBT) is difficult due to the rarity of these lesions and the lack of presenting signs and symptoms. This fact may delay the treatment and therefore worsen the outcome [1]. The small bowel represents approximately 75 percent of the length and over 90 percent of the surface of the alimentary tract; however small bowel malignancies represent only 3 percent of all gastrointestinal tract neoplasms [2,3]. The MSBT histologic type incidence distribution is carcinoids (44%), adenocarcinomas (33%), stromal tumors (17%) and lymphomas (8%) [1]. Their pathogenesis is unknown, but risk factors such as hereditary cancer syndromes, chronic inflammation (inflammatory bowel disease), dietary factors, tobacco and obesity should be considered [4,5]. The most common presenting symptom is abdominal pain, typically intermittent and crampy. Weight loss, nausea and vomiting, gastrointestinal bleeding and intestinal obstruction are reported [6,7]. As compared to benign tumors, patients with MSBT are more often symptomatic, even though, the delay between onsets of symptoms to diagnosis may be up to 30 weeks [6]. As a result, by the time the diagnosis is made, the disease is usually advanced, with either regional or distant metastasis. Exploratory laparotomy is the most sensitive diagnostic modality in evaluating a patient with a high suspicion of having a small bowl neoplasm [8].
Materials and Methods
6 cases of MSBT were operated by Clinica Reis Neto staff (Campinas, SP, Brazil) from 2015 to 2017. Their medical records were reviewed retrospectively and presented after informed consent was signed by all six patients.
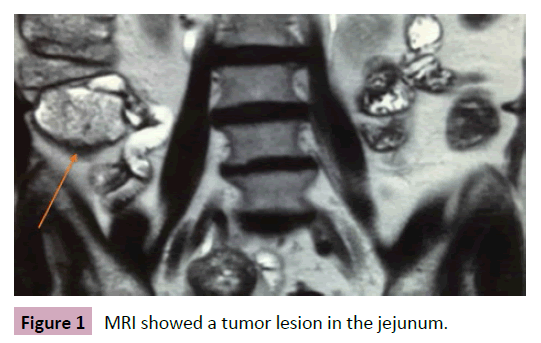
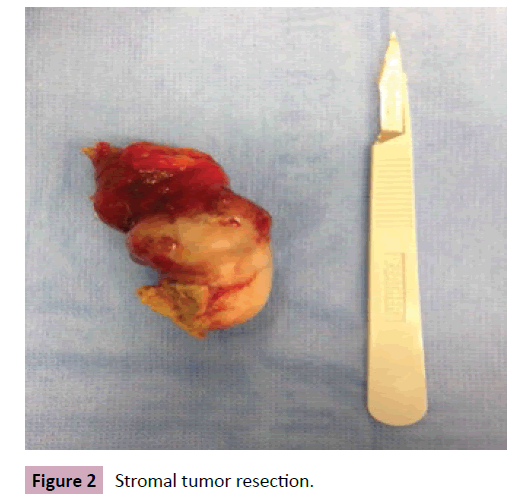
Case #1 presentation
66-year-old patient presented with bloody diarrhea, abdominal cramp and stool thinning for the past 2 months. There was no history of fever or weight loss and physical examination was clear. Colonoscopy of no significance. Computed tomography (CT) and magnetic resonance image (MRI) showed a tumor lesion in the jejunum (Figure 1). The patient was submitted to a laparoscopic enterectomy with end to end anastomosis (Figure 2). The intra operatory showed advanced disease to the peritoneum, locally, due to extra luminal involvement. The patient had a good outcome and was discharged after three days. The pathology showed a low-grade 4 centimeters stromal tumor (positive CKit and less than 5 mitoses per 50 fields). The patient was sent to Oncology, received Imatinib chemotherapy and after two years of follow up she has no signs of recurrence.
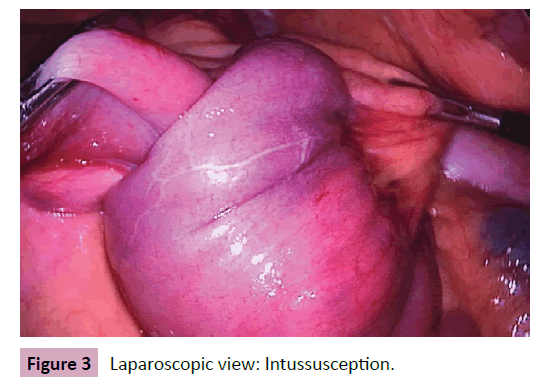
Case #2 presentation
51-year-old female with intermittent general abdominal pain and melena. Presented a normal endoscopy and colonoscopy. CT scan showed intussusception of the proximal jejunum to the duodenum. Laparoscopic surgery was performed with a 20-centimeter enterectomy. Pathology confirmed a stromal tumor (positive cKit, low grade) (Figures 3 and 4). The patient did not need post operatory chemotherapy and is disease free after 8 months.
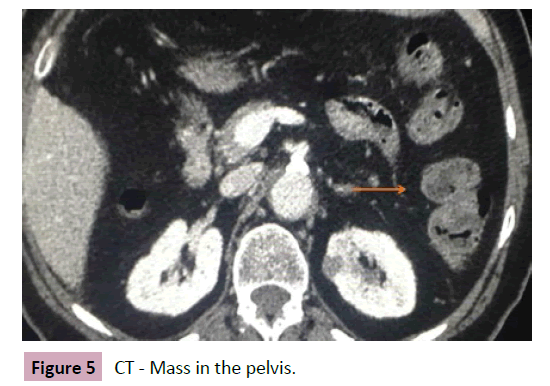
Case #3 presentation
74-year-old woman presented abdominal pain for 3 months. During investigation, ultrasound and CT scan evidenced a small hypoechoic lesion in the pelvis. Patient was submitted to exploratory laparotomy by the gynecology staff. During surgery a small bowel tumor was found in the jejunum and a 10 centimeters enterectomy was performed. The postoperative pathology showed a high-grade stromal tumor (cKit positive and more than 5 mitoses per 50 fields). The patient was submitted to Imatinib chemotherapy (Figures 5 and 6).
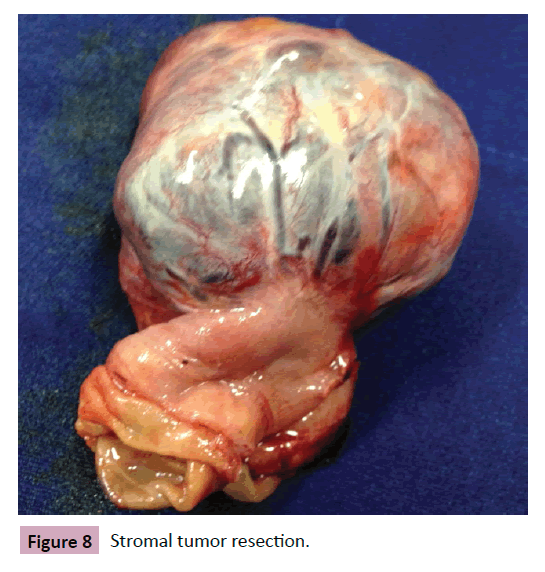
Case #4 presentation
70-year-old patient with melena episodes for 1 year. Hospitalized previously with hemodynamic instability, requiring blood transfusion. Had a medical history of rheumatic cardiopathy, arterial hypertension and hypothyroidism. Colonoscopy and endoscopy were clear, however MRI showed a tumor in the jejunum (Figure 7). Enterectomy was performed and pathology defined a stage 1, low-grade stromal tumor (5 cm, cKit positive, 3 mitoses/50 field) (Figure 8).
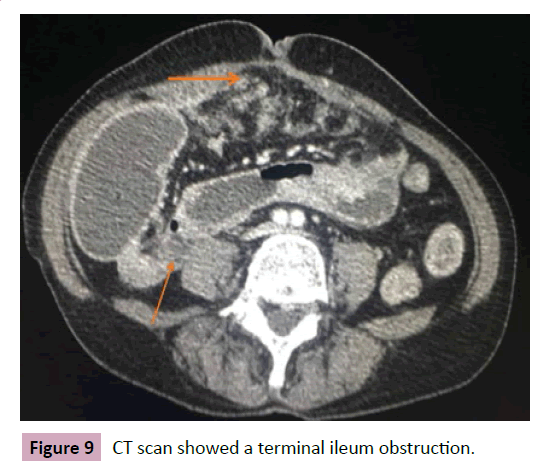
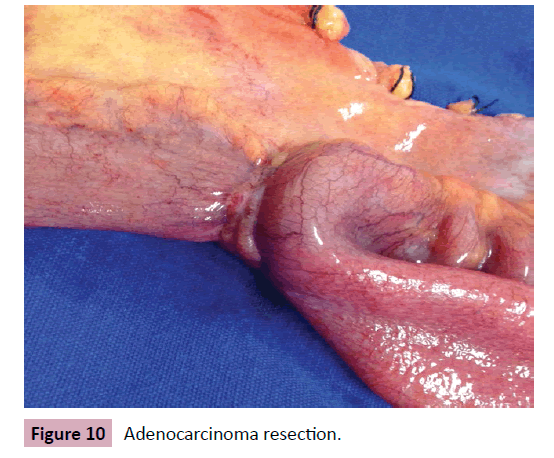
Case #5 presentation
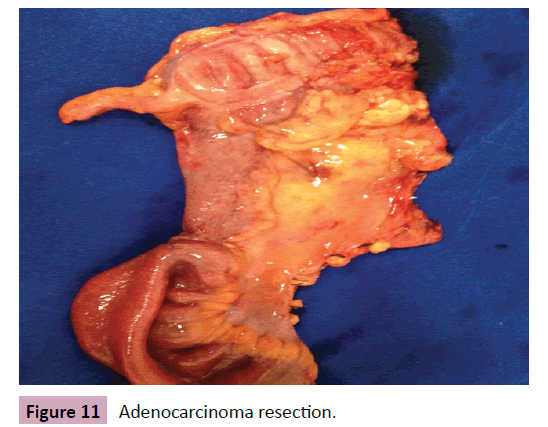
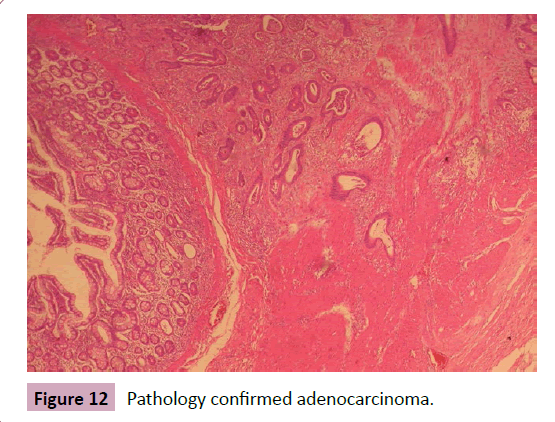
57-year-old patient presented diffuse abdominal pain, abdominal distension, weight loss, nausea and vomiting for 2 months. No comorbidities or family history worth noting. At physical examination important weight loss and abdominal distension, with no signs of peritonitis. CT scan showed an obstructive area in the terminal ileum with no significant distension (Figure 9). Exploratory laparotomy was performed with terminal ileum-right colectomy with ileotransverse anastomosis due to stenotic lesion (Figures 10 and 11). Pathology showed a stage III adenocarcinoma (Figure 12). The patient was referred to the Oncology center and underwent chemotherapy.
Case #6 presentation
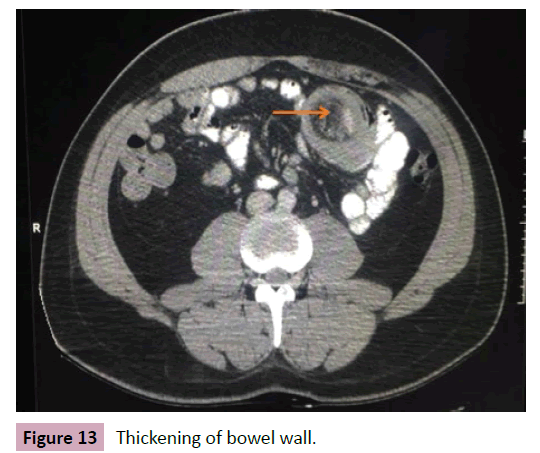
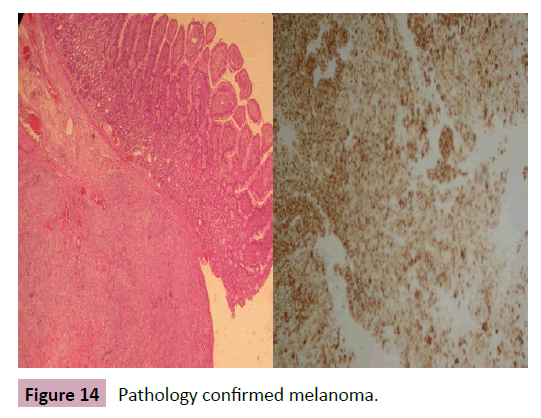
32-year-old male reported with epigastric colic pain, fecal dryness, with melena, without frequency alteration for 10 days. CT scan showed thickening of the bowel wall (Figure 13). Colonoscopy stopped at splenic angle duo to sharp angulation. As patient did not improve clinical picture, exploratory laparotomy was performed and found the presence of 3 small bowel intraluminal tumors at 15, 40 and 190 centimeters of Treitz angle. Enterectomies were performed and pathology reported amelanotic malignant melanoma (Figure 14). Patient started chemotherapy for metastatic melanoma, however two months later presented a left axillary tumor, also confirmed as metastatic melanoma. Chemotherapy was performed however patient died after 4 months.
Results
Six cases of MSBT were analyzed, one metastatic and five of primary origin. In five patients (83.3%) the lesion was in the jejunum and one (16.7%) was in the ileum. Diagnostic confirmation was performed by surgical approach and histological study. The procedures adopted included: segmental enterectomy with lymphadenectomy in all six cases. One patient had a right colectomy with transverse ileus anastomosis and another case had a peritoneal resection due to peritoneal metastasis. There were no anastomosis leak and the average hospitalization time was 4 days. The pathological study of the resected specimens identified four stromal tumors (66.6%), one adenocarcinoma (16.7%) and one metastatic melanoma (16.7%). Five cases underwent chemotherapy. One patient died after four months due to metastatic disease (Metastatic melanoma case) and the other five are disease free.
Discussion
Malignancies involving the small intestine are rare and account for less than 3% of the gastrointestinal tract cancers [9]. The most common histological type is the carcinoid. However, this limited sample showed a higher incidence of stromal tumors. When the different regions of the intestine are considered, adenocarcinomas are mostly found in the duodenum while stromal tumors are usually spread throughout the entire small bowel [9]. Adenocarcinoma represents 33% of MSBT. They usually present between the ages of 50 to 70, with a male predominance. The risk for small bowel adenocarcinoma is higher in patients with chronic inflammation such as Crohn’s disease and in colorectal cancer [10,11]. The presenting symptoms are vague, such as abdominal pain, nausea and anemia. Therefore, most cases are diagnosed in an advanced stage (58% are stage III and IV at diagnosis) [10,11]. Localized adenocarcinoma is best managed with wide segmental surgical resection and primary and regional node lymphadenectomy. When located at the distal ileum must be treated with right colectomy that includes resection of the ileocolic artery [11]. Adjuvant therapy is indicated to lymph nodepositive [12,13]. Sarcomas represent 17% of MSBT. The most common type of intestinal sarcoma is a gastroduodenal stromal tumor (GIST), accounting 83% of the cases [14]. They usually present with abdominal pain, weight loss, bleeding and palpable mass. As they tend to enlarge extraluminally, obstruction is rare [14]. The primary treatment modality is en bloc segmental resection with tumor-free margins, with preservation of the tumor’s pseudocapsule. Small molecule tyrosine kinase inhibitors such as Imatinib can be used for adjuvant and neoadjuvant treatment [14]. Secondary neoplastic involvement of the small intestine is more common than primary small neoplasia [15]. That can happen by extraluminal involvement, erosion through the bowel wall or hematogenous spread. The small bowel is the most frequent site of gastrointestinal metastases in metastatic melanoma [15]. The treatment of theses lesions is palliative and procedures, such as limited resection or bypass, should be reserved to relieve symptoms [15].
Conclusion
MSBT have a rare incidence, however attention and investigation of persistent symptoms may lead to an early diagnosis and treatment.
References
- Weiss NS, Yang CP (1987) Incidence of histologic types of cancer of the small intestine. J Nat Cancer Inst 78: 653-656.
- Raghav K, Overman MJ (2013) Small bowel adernocarcinomas-existing evidence and evolving paradigms. Nat Rev Clin Oncol 10: 534-544.
- Siegel RL, Miller KD, Jemal A (2018) Cancer statistics 2018. CA Cancer J Clin 68: 7-30.
- Chow WH, Linet MS, McLaughin JK, Hsing AW, Chien HT, et al. (1993) Risk factors for small intestine cancer. Cancer Causes Control 4: 163-169.
- Billimoria KY, Bentrem DJ, Wayne JD, Ko CY, Bennett CL, et al. (2009) Smal bowel cancer in the United States: changes in epidemiology, treatment, and survival over the last 20 years. Ann Surg 249: 63-71.
- McLaughin PD, Maher MM (2013) Primary malignant diseases of the small intestine. AJR Am J Roentgenol 201: W9.
- Neugut AI, Jacobson JS, Suh S, Mukherjee R, Arber N (1998) The epidemiology of cancer of the small bowel. Cancer Epidemiol Biomarkers Prev 7: 243-251.
- North JH, Pack MS (2000) Malignant tumors of the small intestine: a review of 144 cases. Am Surg 66: 46-51.
- Bruneton JN, Droullard J, Bourry J, Roux P, Lecomte P (1983) Adenocarcinoma of the small intestine. Current state of diagnosis and treatment. A study of 27 cases and a review of the literature. J Radiol 63: 117-123.
- Overman MJ, Hu CY, Kopetz S, Abbruzzese JL, Wolff RA, et al. (2012) A population-based comparison of adenocarcinoma of the large and small intestine: insights into a rare disease. Ann Surg Oncol 19: 1439-1445.
- Young JI, Mongoue-Tchokote S, Wieghard N, Mori M, Vaccaro GM, et al. (2016) Treatment and survival of Small-bowel adenocarcinoma in the United States: A Comparison with colon cancer. Dis Colon Rectum 59: 306-315.
- Ciresi DL, Scholten DJ (1995) The continuing clinical dilemma of primary tumors of the small intestine. Am Surg 61: 698-702.
- Sohn TA, Lillemoe KD, Cameron JL, Pitt HA, Kaufman HS, et al. (1998) Adenocarcinoma of the duodenum: factors influencing long term survival. J Gastrointest Sur 2: 79-87.
- Maglinte DD, OÇonnor K, Bessette J, Chernish SM, Kelvin FM (1991) The role of the physician in the late diagnosis of primary malignant tumors of the small intestine. Am J Gastroenterol 86: 304-308.
- Cunningham JD, Aleali R, Aleali M, Brower ST, Aufses AH (1997) Malignant small bowel neoplasms: histopathologic determinants of recurrence and survival. Ann Surg 225: 300-306.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences