Successful Endoscopic Management of Colonic Cavernous Vascular Malformation: A Rare Cause of Hematochezia
Ligeiro FA, Twaddell W, Xie G and Quezada SM
DOI10.21767/2471-9943.100037
Ligeiro FA1, Twaddell W2, Xie G1 and Quezada SM1*
1Division of Gastroenterology and Hepatology, University of Maryland School of Medicine, Baltimore, USA
2Department of Pathology, University of Maryland School of Medicine, Baltimore, USA
- *Corresponding Author:
- Quezada SM
Division of Gastroenterology and Hepatology
University of Maryland School of Medicine
Baltimore, USA
Tel: 14103285780
E-mail: squezada@som.umaryland.edu
Received date: April 13, 2017; Accepted date: April 27, 2017; Published date: May 02, 2017
Citation: Ligeiro FA, Twaddell W, Xie G, et al. Successful Endoscopic Management of Colonic Cavernous Vascular Malformation: A Rare Cause of Hematochezia. Colorec Cancer. 2017, 3:1. doi: 10.21767/2471-9943.100037
Copyright: © 2017 Ligeiro FA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Despite approaching 200 years since they were first documented to exist, cavernous vascular malformations of the gastrointestinal tract remain exceedingly rare. To date about 350 cases have been reported [1]. Unlike hemangiomas, which are associated with high endothelial cell turnover, cavernous malformations occur under normal endothelial conditions [2]. When found, these rare entities are more often identified in the small bowel; colonic lesions are even more evasive. Although approximately 80% of these lesions present with hematochezia, they often go misdiagnosed as hemorrhoids, or inflammatory bowel disease. Traditionally, surgical resection is considered the standard approach for management of these lesions, but in a few cases, endoscopic resection has been successful. We present here a case of successful endoscopic resection of a large, bleeding colonic vascular malformation in a patient with HIV.
Case
The patient was a 38 year old African-American male with HIV on antiretroviral therapy, and multiple potential risk factors for hematochezia including prior Shigella infection, remote family history of colon cancer and receptive anal intercourse, who presented with a one year history of intermittent rectal bleeding. He described associated urgency and rectal pain, though denied abdominal pain or weight loss. He had never undergone colonoscopic evaluation in the past.
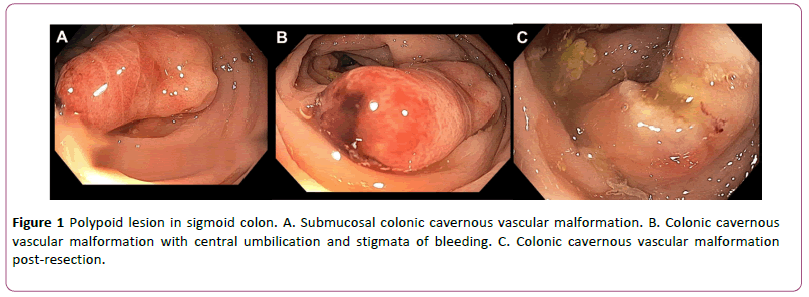
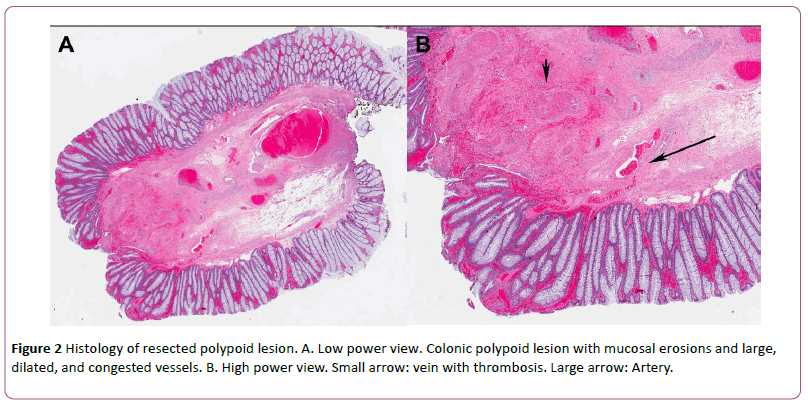
At the time of his first clinical examination his vitals were noted to be within normal limits, without evidence of tachycardia or hypotension to suggest volume depletion. Other than a thin frame, his physical exam was also normal, without evidence of cutaneous vascular lesions and no abdominal tenderness to palpation was elicited. His laboratory examination was notable for a hemoglobin of 15.1 g/dL, MCV 93, and his iron panel was normal with an iron level of 70 mcg/dL, and a ferritin of 22 ng/dL. There was no evidence of inflammatory marker elevation, such as in ESR or CRP. He was recommended to undergo colonoscopy for evaluation of hematochezia, and this was notable for large internal hemorrhoids, and an approximately 10 mm diameter by 20 mm in length pedunculated polypoid lesion in the sigmoid colon (Figure 1A). The lesion was noted to have a submucosal appearance in that the overlying mucosa appeared smooth and normal, with exception of progressively more erythematous discoloration toward the tip of the lesion. The lesion also contained a central umbilication with pinpoint ulceration and overlying adherent hematin, consistent with stigmata of recent bleeding (Figure 1B). There were no other abnormalities seen in the colon. At the base of the polypoid lesion, there was no erythema and the mucosa appeared normal. This was deemed to be the cause of the patient’s hematochezia given the overlying stigmata, and the lesion was completely removed with snare cautery polypectomy without adverse events, and there was no bleeding at the end of the procedure (Figure 1C). Histopathology was consistent with a submucosal vascular malformation with ulceration and reactive changes (Figure 2A and 2B). No evidence of Kaposi’s sarcoma or other malignancy was noted within the lesion.
The patient was followed closely and confirmed there was no recurrence of bleeding 24 hours after the procedure, and remained stable on follow-up two weeks after the resection. He was later lost to follow-up.
Discussion
Colonic submucosal vascular malformations are rare causes of hematochezia. To date, about 350 cases have been reported worldwide [3]. Due to the paucity of these lesions, and the variability in appearance, diagnosis is often delayed and especially when presenting with mucosal edema, nodularity and vascular congestion, they may be mistaken for inflammatory bowel disease. While epidemiologic data for these malformations is sparse, it is understood that the colonic location seems to affect men and women equally [4]. Our patient had a prior history of HIV, which is associated with Kaposi sarcoma, vascular cutaneous or mucosal malignant lesions which also arise from the endothelium. In the gastrointestinal tract, these Kaposi sarcomas can also present as polypoid lesions that protrude into the lumen, and have been documented as having umbilication and ulceration, making Kapsoi sarcoma part of the differential diagnosis for this lesion [5]. That said, highly active anti-retroviral therapy, which our patient was taking, is considered protective against these Kaposi sarcomas [6]. At this time, there are no known associations between antiretroviral therapy and colonic cavernous vascular malformations.
Biopsy is not recommended given the risk of bleeding, which may present a diagnostic challenge. Surgery can be a definitive diagnostic and therapeutic strategy [1], however in appropriate cases such as this one, endoscopic resection with cauterization can also be successful, and may present a reasonable conservative option, particularly in those who may not be ideal candidates for surgery.
References
- Yoo S (2011) GI-Associated hemangiomas and vascular Malformations.Clin Colon Rectal Surg 24: 193–200.
- Mallucci P (1999) Vascular anomalies must be properly classified.BMJ 319:919.
- Kimura S, Tanaka S, Kusunoki H, Kitadai Y, Sumii M, et al. (2007) Cavernous hemangioma in the ascending colon treated by endoscopic mucosal resection. J Gastro Hep 22:280–281.
- Gentry RW, Dockerty MB, Glagett OT (1949) Vascular malformations and vascular tumors of the gastrointestinal tract.SurgGynecolObstet 88:281–323.
- Clin Colon Rectal Surg
- Antman K, Chang Y (2000) Kaposi's Sarcoma.NEJM342: 1027–1038.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences