The Surgical Technique of Hand-Assisted Laparoscopic Sigmoid Colectomy
Abdul-Wahed Nasir Meshikhes
Abdul-Wahed Nasir Meshikhes*
Section of General and Minimally Invasive Surgery, Department of Surgery, King Fahad Specialist Hospital, Dammam 31444, Eastern Province, Saudi Arabia
- *Corresponding Author:
- Abdul-Wahed Nasir Meshikhes
FRCSI, FACS, Section of General and Minimally Invasive Surgery, Department of Surgery, King Fahad Specialist Hospital, Dammam 31444, Eastern Province, Saudi Arabia
Tel: +966-844 2222
E-mail: meshikhes@gmail.com
Received date: February 03, 2016; Accepted date: February 19, 2016; Published date: February 25, 2016
Citation: Meshikhes AW. The Surgical Technique of Hand-Assisted Laparoscopic Sigmoid Colectomy. Colorec Cancer 2016, 2:1. doi: 10.21767/2471-9943.100015
Abstract
Hand assisted laparoscopic surgery (HALS) was introduced to overcome the challenging issues of totally laparoscopic procedures. It combines the advantages of open surgery - with the surgeon's non-dominant hand inside the abdomen–as well as those of minimally invasive techniques. A hand inside the abdomen does restore the tactile feedback sensation-which is lacking in laparoscopic surgery-, allows safe finger dissection and retraction, and improves hand-eye coordination. The author introduces HAL colectomy as a bridge towards totally laparoscopic colorectal surgery. This article describes how hand assisted sigmoid colectomy is performed.
Keywords
Hand-assisted surgery; Laparoscopy; Colorectal surgery; Colectomy; Colon cancer
Introduction
Although the first reported laparoscopic assisted colectomy was in 1991 [1], the number of laparoscopic colonic procedures remained a minority of colonic resections. This was attributed to the fact that laparoscopic colectomy is technically challenging and demands a long learning curve. Therefore, hand-assisted laparoscopic surgery (HALS) was advocated as a useful alternative to laparoscopic colonic surgery and was introduced as a hybrid technique that allows the introduction of the surgeon's nondominant hand into the abdomen through a special hand port while maintaining pneumo peritoneum [2]. This permits laparoscopic visualization, assists in dissection, retraction and placement of laparoscopic instruments. In this respect, HALS combines the advantages of open surgery-with the surgeon's non-dominant hand inside the abdomen-and those of minimally invasive techniques. A hand inside the abdomen does restore the tactile feedback sensation-which is lacking in laparoscopic surgery-, allows safe finger dissection and retraction, and improves hand-eye coordination. All those factors may play an important part in reducing the operative time [3].
HALS is further advocated in laparoscopic procedures that require an incision to retrieve the resected specimen as in colonic resection. Such an incision which is usually made at the end of laparoscopic procedures may well be utilized earlier at the beginning of the operation to place a hand port that allows the surgeon to pass his/her non-dominant hand to facilitate dissection and thereby reduce the operative time [3-5].
The technique of hand-assisted laparoscopic (HAL) sigmoid colectomy is described here as an example of hand-assisted laparoscopic surgery. This technique was introduced as a ‘bridge’ towards totally laparoscopic colorectal surgery.
Indications for sigmoid colectomy
The indications for hand-assisted laparoscopic sigmoid colectomy are similar to those of conventional open method. The technique can be offered to all new comers with any sigmoid pathology that requires resection. Most common indications in the author's region are sigmoid tumours either benign or malignant, sigmoid volvulus and less commonly diverticular disease.
Preoperative preparation
Routine preoperative blood investigations, chest x-ray and ECG are performed. Staging workup includes computerized tomography scan (CT) of the chest, abdomen and pelvis, colonoscopy and biopsy of the lesion to confirm the diagnosis. It is preferable to prepare two units of packed red blood cells. Although preoperative bowel preparation for colonic surgery is greatly debated, mechanical bowel preparation is usually given as early as possible on the day before surgery to avoid gaseous bloating of the colon which may create technical difficulties during the operative procedure.
In patients with sigmoid adenocarcinoma, if the tumour is not visible on the CT scan it is advisable to tattoo the tumour with India ink at colonoscopy before surgery. This is especially of vital importance if laparoscopic-assisted and not hand-assisted colectomy is to be performed. Anti-DVT prophylaxis in the form of low molecular weight heparin is also prescribed and prophylactic antibiotics are administered in the operating room during induction of anaesthesia. The combination of cefuroxime 750 mg and metronidazole 500 mg is given as a single dose in most cases. In some cases, further two doses are given at 8 and 16 hours postoperatively.
Instruments Needed
A number of instruments are needed to perform a successful hand assisted laparoscopic colectomy:
• Hand port: the author was trained to use Lap Disc (Ethicon Endosurgery, Cincinnati, Ohio, USA). The size needed (small, medium or large) depends on the patient's abdominal wall thickness and contour. The Lap Disc consists of three overlaid plastic rings interconnected by a silicone rubber membrane (Figure 1). The bottom flexible ring has a memory that allows it to be inserted snugly into the abdominal cavity. The two rigid upper and middle rings lock together via a sliding gear and are twisted to close clockwise to maintain peritoneal gas pressure, creating what is called 'the iris valve' aperture of which can be continuously adjusted. Excessive tightness of the aperture should be avoided. To open the disc, the upper ring is lifted and slightly rotated clockwise first to release the gears then slowly rotate anticlockwise.
• Electrosurgical generator: whether to use the Harmonic Scalpel (Ethicon Endosurgery, USA) or the Ligature (Tyco, USA) is entirely dependent on the surgeon's own preference and discretion.
• Two to three disposable 12 mm and 10 mm trocars.
• Endo staplers (Ethicon Endosurgery, Cincinnati, Ohio, USA): two 45 mm endoscopic articulating linear cutter with vascular reloads and blue reloads.
• Circular staplers of open surgery.
Procedure
Position of patient and operating room setup
Under general anaesthesia with endotracheal intubation, the patient is laid supine on the table with both arms tucked at the sides to allow more room for the surgeon and assistant to move. Patient's legs are laid flat and separated to facilitate transanal passage of the circular staplers for colo-rectal anastomosis at a later stage of the procedure. This obviates the need for Lloyd- Davies position which may not be necessary. Once anaesthesia is induced, a naso-gastric tube and a urinary catheter are inserted, both of which may be removed at the end of the operation.
The primary surgeon stands on the patient's right side and his assistant/camera man on the left side of the patient. The two monitors (primary and secondary) are placed at the side of patient's legs to allow both surgeon and assistant the best and optimal screen views.
Placement of the hand port
After preparation of the abdomen and perineum with sterilizing solution, the abdomen and legs are toweled. A vertical mid-line incision (4 fingers breadth) is marked as the site of the hand port insertion. This 6-7 cm mid-line incision which out-skirt the umbilicus is deepened through the linea alba and peritoneum to the abdominal cavity. Haemostasis is secured with diathermy. Two stay sutures are placed and attached to haemosatic clips to allow lifting of the abdominal wall during insertion of the hand port and later to facilitate the repeated introduction of the surgeon's nondominant hand. Care must be taken not to touch the hand port with the clips. The hand port is inserted by pushing the flexible ring slowly into the abdominal cavity after lifting up abdominal wall using the stay sutures on that side. The other stay suture is then lifted and the flexible ring is slowly and gently pushed into the abdominal cavity. Full sealed contact between the flexible ring of the disc and the anterior abdominal wall is secured. The lap disc aperture is tightened clockwise around a 10-11 mm trocar and pneumoperitoneum is induced by insufflating the abdomen with CO2 to 13-15 mmHg.
Placement of trocars
A 12 mm trocar is inserted in the right flank or in the right iliac fossa to allow passage of harmonic scalpel, other dissectors and endopath staplers. Another 10-11mm trocar is inserted in the suparpubic area over the midline for the camera. Occasionally a third 10 mm port may be needed in the left flank at the level of umbilicus to be used as another port for the camera. Although 300 camera laparoscope is ideal in laparoscopic colectomy, 00 camera is just as good in providing adequate views (Figure 2).
The procedure
Once the port site is inserted and aperture is tightened around a 10 mm trocar, pneumoperitoneum is induced and the laparoscope is passed. The other 2-3 trocars were inserted in the positions indicated above under direct vision. Now the abdominal cavity is thoroughly inspected using the laparoscope. The trocar is then removed and the inside of the disc is lubricated using sterile k-y jelly. The lubricated back of the surgeon's non-dominant (left) hand is inserted through the port aperture into the abdominal cavity. The abdominal organs especially the liver, lymph nodes and the entire colon are thoroughly palpated and the site of the pathology is identified. The patient is then placed in a steep Trendelenberg position and tilted to the right to allow gravity displacement of small bowel loops to the right upper quadrant with subsequent exposure of the surgical field.
After confirming the site of the pathology, lateral to medial dissection of the descending and sigmoid colons is commenced by using the hand to retract the colon medially and the harmonic scalpel or a dissector to open the lateral peritoneal reflection at the white line of Toldts. A mixture of blunt and sharp dissection using the left hand and harmonic scalpel through the second port may be needed. As left colon is fully mobilized medially, the left ureter and gonadal vessels must be identified before proceeding any further. The dissection is continued all the way up along the descending colon until the splenic flexure and down as far as upper rectum. The colon is then reflected laterally using the hand to allow visualization of the left colon and sigmoid mesentery which if put under stretch, the inferior mesenteric vessels stands out for easy identification. This vascular pedicle is dissected with its accompanied lymph nodes using the harmonic scalpel and is best-divided using vascular endostaplers or by Ligasure vessel sealer if available.
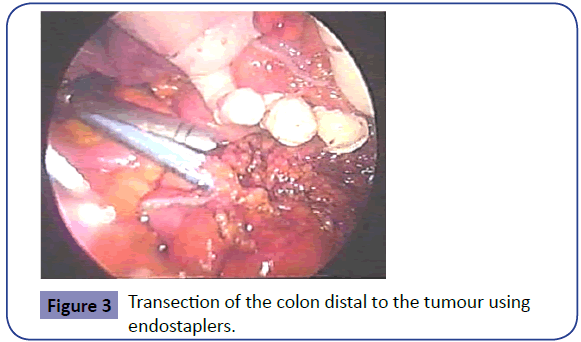
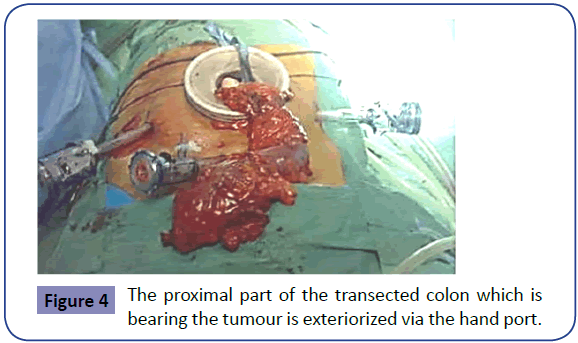
The medial dissection of the mesentery is then continued in the plane anterior to Gerota fascia in a similar fashion using the harmonic scalpel to seal smaller mesenteric vessels. This continues until the haematoma of the lateral dissection is apparent and the sites of anticipated proximal and distal resections are reached. Endostaplers with blue reloads are then passed through the second trocar and used to transect the rectosigmoid colon distally (Figure 3). The transected proximal end is then brought out to the exterior via the lap disc, which is left in situ as a protective cover to the wound (Figure 4). The proximal end is transected after application of a soft non-crushing bowel clamp and the specimen is sent for histopathology.
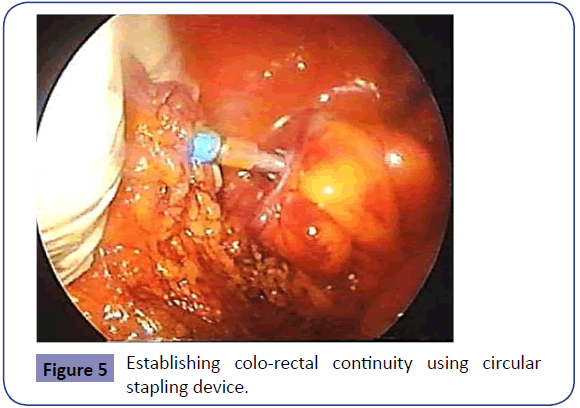
The anvil of a circular stapler size 29 or 31 is placed in the distal end of the colon and a purse-string suture is made over it. The purse-stringed end of the colon with the anvil is introduced back into the peritoneal cavity. The left hand is also inserted and the abdomen is insufflated again. The end of the descending colon with the anvil is held and oriented after the identification of the rectal stump.
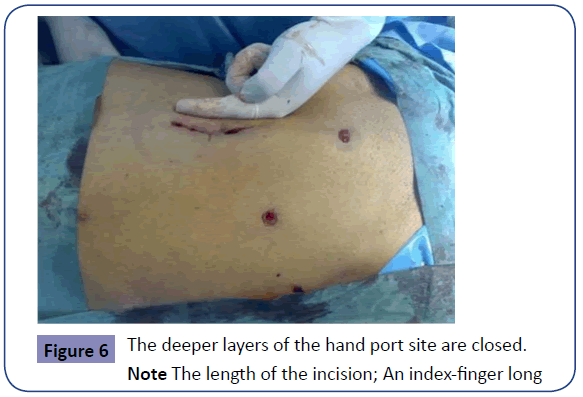
The doubly gloved right hand of the primary surgeon is then used to introduce the circular stapler per anus after an assistant performs a sphincter stretch. Under laparoscopic vision, the anvil is attached to the trocar of the circular stapler while maintaining anatomical mesenteric alignment (Figure 5). The circular stapler is closed -after making sure no other structures are enclosed- and fired using double stapling technique creating the end-to-end colo-rectal anastomosis. The stapling device is then withdrawn and the doughnuts are tested for completion before sending them and the resected portion of the colon for histopathology. The integrity of the anastomosis is tested by filling the pelvis with sterile water and insufflating air through the anus using a bladder syringe or a rigid sigmoidoscope. The paracolic gutter is finally inspected for any bleeding, which should be secured. Depending on the discretion of the surgeon, a suction drain may be inserted in the pelvis or in the paracolic gutter via the hypogastric or the left flank port site. The abdomen is fully deflated before all trocars are removed and fascial sutures are inserted at all trocar sites to avoid development of future trocar hernias. After removal of the port site, a mass closure of the mid-line wound is performed (Figure 6).
Postoperative care
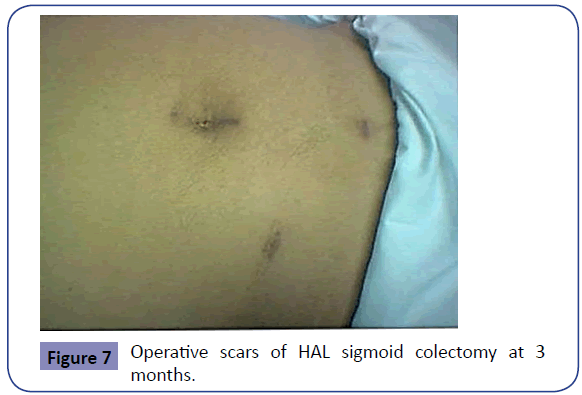
A shared advantage with laparoscopic colectomy, HALS is associated with decreased postoperative narcotic use [6]. Hence, intramuscular analgesia is prescribed for 24-48 hours only. This is later shifted to oral non-steroidal anti-inflammatory analgesia. The patient is allowed sips of water by mouth once fully recovered and free oral fluids are given on the first operative day. Soft diet is given on the second day and on the third day full diet is resumed. Drain if inserted is removed when contents are minimal; usually by second or third day and the patient is discharged on the 4th or 5th postoperative day if no complications developed. The cosmetic result of the procedure is very acceptable and satisfying especially to female patients (Figure 7).
Discussion
HALS has been used for segmental resection of the colon, anterior resections, total colectomy, reversal of Hartmann procedure, and rectal procedures such as rectopexy, and abdominoperineal resection. Its advantages over the laparoscopic-assisted colectomy include the easier exploration, dissection, and colonic mobilization, and better control of hemorrhagic accidents, thus reducing the conversion rate.
There is no doubt that HALS colorectal surgery is far superior to open colectomy (OC) as it preserves the advantages of minimally invasive surgery. A randomized controlled trial (RCT) that compared two well matched groups of patients undergoing elective right colonic cancer resections (HALS vs. open) found that HALS took significantly longer time to perform, but resulted in significantly less blood loss and was associated with significantly less pain [7]. Moreover, patients in the HALS group recovered faster, and had a shorter length of hospitalization. In another RCT, HALS was associated with significantly shorter hospital stay and incision length, faster recovery of gastrointestinal function, less analgesic requirement and blood loss, and lower pain scores. Moreover, there were no significant differences in operating time, complications, or time to full recovery [8].
Several studies were published in the literature comparing HALS to laparoscopic assisted colorectal procedures; some were RCTs [9-12], and others were prospective non-randomized studies [13,14]. The HALS study found no significant difference between the two groups in term of operating time, length of incision, complication rate and length of hospital stay. However, there were fewer conversions in the HALS group [9]. Targarona et al. found the operating time and clinical outcome were similar, but, the conversion rate was much higher in the laparoscopic group [12]. However, 4 of 6 conversions in the laparoscopic group were completed with the hand-assisted technique. Similarly, the Minimally Invasive Therapy and Technology (MITT) group study found no significant difference in the complication rate and long-term clinical outcome, but the conversion rate was lower in the HALS group [11]. Moreover, there were no apparent differences in the time for bowel function recovery, tolerance of diet, length of hospital stay, postoperative pain scores, or narcotic use between the two groups [11]. Tjandra et al. found similar oncological harvest in term of tumor clearance and number of lymph nodes retrieved between the two groups [13]. But, the operating time was significantly shorter in the HALS group. Also, the bowel function recovery and flatus passage were delayed in the HALS group. Hence, this study has shown some difference in recovery in favor of the laparoscopic group [14]. A large retrospective single institution study from the Lahey clinic comparing hand assisted sigmoid colectomy (n = 66) with laparoscopic sigmoid colectomy (n = 85) revealed no significant difference in bowel function recovery (2.5 d vs 2.8 days), length of hospital stay (5.2 d vs 5.0 days) or short-term complications such as anastomotic leak, ileus and wound infection (21% vs 23%) between the two groups [15]. However, there was significant difference in the operating time (189 min vs 203 min) and conversion rate (0% vs 13%) in favor of the HALS group. The incision length was, however, significantly smaller (8.1 cm vs 6.2 cm) in the laparoscopic group [15]. Based on the reviewed literature, the following can be concluded when comparing HALS and laparoscopic colorectal surgery:
• HALS offers similar minimally invasive benefits as laparoscopic approach with a shorter operative time and lower conversion rate.
• Both approaches have comparable complication rate and length of stay, but the incision length is bigger in HALS.
• There is an increased level of inflammatory markers with an increased need for postoperative narcotics analgesia and delayed bowel function recovery after HALS.
• However, HALS is more suitable for obese patients and in lengthy operative procedures such as total colectomy.
The author has used HALS in colorectal surgical procedures as a bridge towards totally laparoscopic surgery .The procedure was easy to learn, easy to teach and can be used as an ‘adjunct’ to laparoscopic surgery. The author now uses totally laparoscopic colorectal procedures for all new comers and hand-assisted surgery is only used if difficulties are encountered or to speed up the procedure. As all the controversial issues surrounding hand assisted colorectal surgery have been addressed [2], HALS procedure can be considered as an extra armamentarium in the hand of laparoscopic surgeons performing colorectal procedures.
Conclusion
HAL sigmoid colectomy combines the advantages of laparoscopic (minimally invasive) as well as that of conventional open surgery with restoration of tactile feedback sensation, safe finger dissection and rapid control of bleeding accidents. As an abdominal wound is needed at the end of totally laparoscopic colectomy procedure for specimen retrieval, this access may well be made and utilized early in the course of the procedure thereby facilitating dissection and reducing the operating time. With this hybrid procedure, the learning curve is very short as most of the technical problems-such as handling the long colon and multiple large vessels ligation-that are associated with laparoscopic colectomy are overcome. Hand assisted laparoscopic surgery is recommended as an adjunct to and a ‘bridge’ towards totally laparoscopic procedures.
Conflict of Interest
The author has no conflict of interest or financial disclosure to declare. However, the author conducted hand assisted laparoscopic surgery workshops which were sponsored by Ethicon Endosurgery (Johnson and Johnson Middle East).
References
- Cooperman AM, Katz V, Zimmon D, Botero G (1991) Laparoscopic colon resection: A case report. J Laparoendosc. Surg1: 221-24.
- Meshikhes AWN (2010) Controversy of hand assisted laparoscopic colorectal surgery. World J Gastroenterol16:5662-8
- Targarona EM, Gracia E, Rodriguez M, Cerdan G, Balague C,et al. (2003)Hand assisted laparoscopic surgery. Arch Surg138:133-141.
- Jakimowicz JJ (2000) Will advanced laparoscopic surgery go hand-assisted? SurgEndosc14: 881-882.
- Katkhouda N, Lord RV (2000) Once more, with feeling: handoscopy or the rediscovery of the virtues of the surgeosn’s hand. SurgEndosc14:985-986.
- Guller U, Jain N, Hervy S, Purves H, Pietrobone R (2003) Laparoscopic vs. open colectomy: outcomes comparison based on large nationwide database. Arch Surg138:1179-86.
- Chung CC, Ng DC, Tsang WW, Tang WL, Yau KK,et al. (2007) Hand-assisted laparoscopic versus open right colectomy: a randomized controlled trial. Ann Surg246:728–733.
- Kang JC, Chung MH, Chao PC, Yeh CC, Hsiao CW,et al. (2004) Hand-assisted laparoscopic colectomy vs open colectomy: a prospective randomized study. SurgEndosc18:577–581.
- HALS Study Group (2000) Hand-assisted laparoscopic surgery vs standard laparoscopic surgery for colorectal disease. SurgEndosc14:896-901.
- Polle SW, van Berge Henegouwen MI, Slors JF, Cuesta MA, Gouma DJ (2008) Total laparoscopic restorative proctocolectomy: are there advantages compared with the open and hand-assisted approaches? Dis Colon Rectum51:541–548.
- Marcello PW, Fleshman JW, Milsom JW, Read TE, Arnell TD,et al. (2008) Hand-assisted laparoscopic vs. laparoscopic colorectal surgery: a multicenter, prospective, randomized trial. Dis Colon Rectum51:818–826.
- Targarona EM, Gracia E, Garriga J, Marti´nez-Bru C, Cortes M,et al.(2002) Prospective, randomized trial comparing conventional laparoscopic colectomy with hand-assisted laparoscopic colectomy: applicability, immediate clinical outcome, inflammatory response and cost. SurgEndosc16: 234-239.
- Tjandra JJ, Chan MK, Yeh CH (2008) Laparoscopic- vs. hand-assisted ultralow anterior resection: a prospective study. Dis Colon Rectum51:26–31.
- Hassan I, You YN, Cima RR, Larson DW, Dozois EJ,et al. (2008) Hand-assisted versus laparoscopic-assisted colorectal surgery: Practice patterns and clinical outcomes in a minimally-invasive colorectal practice. SurgEndosc. 22:739–743.
- Meshikhes AWN, El Tair M, Al Ghazal T (2011)Hand-assisted laparoscopic colorectal surgery: initial experience of a single surgeon.Saudi J Gastroenterol17:16-9.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences