Current Prevalence of HCV in Patients with Liver Disease and its Related Profile
Narayanasamy K, Janifer Jasmine J, Jai Ganesh M, Senthil Kumar R, Koodal Raj A and Muthu Kumaran R
DOI10.21767/2471-9943.100030
Narayanasamy K, Janifer Jasmine J*, Jai Ganesh M, Senthil Kumar R, Koodal Raj A and Muthu Kumaran R
Department of Hepatology, Rajiv Gandhi Government General Hospital, Park Town, Chennai, Tamil Nadu, India
- *Corresponding Author:
- Janifer Jasmine J
Anaerobe Laboratory, Department of Microbiology
Institute of Biomedical Science
University of Sao Paulo, Sao Paulo, SP, Brazil.
E-mail: jasminemercy777@gmail.com
Received Date: November 09, 2016; Accepted Date: December 12, 2016; Published Date: December 18, 2016
Citation: Narayanasamy K, Jasmine JJ, Ganesh MJ, et al. Current Prevalence of HCV in Patients with Liver Disease and its Related Profile. Colorec Cancer 2016, 2:4. doi: 10.21767/2471-9943.100030
Abstract
Background: To study the prevalence of HCV in patients with Liver disease, HCV related patient’s profile, age, obesity, habits, biological marker, Co-morbidities, Diabetes, Obesity, Hepato Celluar Carcinoma (HCC) and detecting Liver stiffness.
Material and methods: Prevalence of HCV was studied in 69,353 patients with liver disease. Tests done and results were recorded.
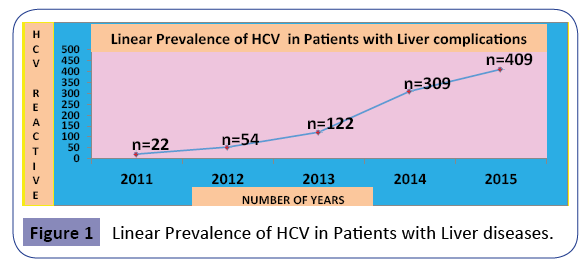
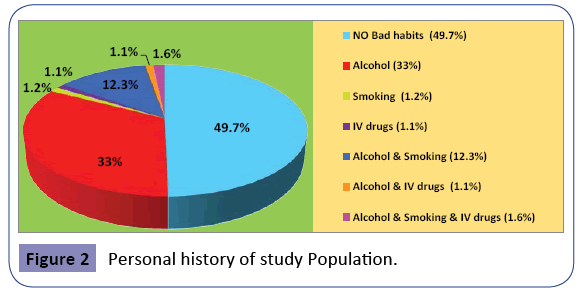
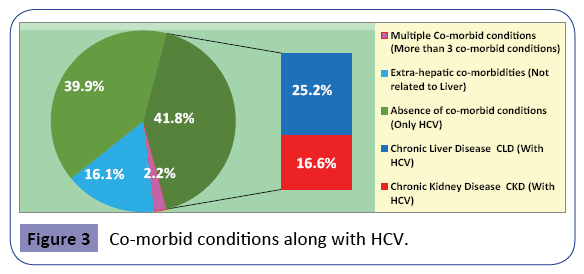
Results: Overall prevalence of HCV in patients with liver disease was 1.3% in our present study, conducted in South Indian population. Statistical significance was found between screened patients and serological and virological reactive patients. Liner prevalence of HCV was observed and double fold increases in the year 2013. No bad habits were found in 49.7% and unhealthy habits in 50.3%. Co-morbidies found in 60.1% and no co- morbidies in 39.9%.
Prevalence of Diabetes mellitus and obese were 20.9% and 34.8% respectively in HCV reactive patients with liver disease. 2.5% of patients were with Hepato Cellular Carcinoma (HCC). Elevation of biological markers were studied (S. protein-63.9%, ALT -50.6%, AST-50.3%. Alkaline phosphatase-(M-35.5%, F-39.1%). As year progresses prevalence of HCV increased in both gender and HCV reactivity were higher in male than female. A statistical significant was found in detecting liver stiffness by fibroscan.
Conclusion: Liner increase of HCV was found. Higher numbers of patients were with unhealthy habits among the study population. CLD and CKD were found in higher percentage in HCV reactive patients with liver disease. 1/5 and 1/3 of our HCV reactive patients were Diabetic and obese respectively. Fibroscan was the best non-invasive marker in detecting liver stiffness in our study.
Keywords
Hepatitis C virus; Chronic liver diseases; Chronic kidney diseases; Co-morbid condition
Introduction
Liver diseases patients seek consultation because of fatigue, loss of appetite, night sweats, low-grade fever, and weight reduction. Some patients show hepatomegaly, abdominal pain, or liver function abnormalities. Disease progression is rapid. Several patients suffer from hepatic encephalopathy early, resulting in coma and even death [1,2]. The radiologic performance of the patient will show that the liver was obviously enlarged and the liver texture was not uniform, combined with patchy low-density shadows [3,4]. Liver diseases double the risk of pathological fractures, regardless of the aetiology of cirrhosis. The total incidence of osteoporosis varies from 12% to 55% [5]. There was a negative impact on renal impairment in patients with liver diseases [6]. Further, the development of cirrhotic cardiomyopathy in up to 40–50% of patients with cirrhosis adds to liver diseases problem [7]. Inflammatory diseases of the liver mainly due to viral infections showed in a study by Ciccone et al. [8]. Hepatitis B virus (HBV) is the most common cause but hepatitis C virus (HCV) is rapidly emerging as an infection requiring attention [9]. HCV is a leading cause of cirrhosis and primary liver cancer [10]. Chronic hepatitis C virus (HCV) infection is a complex, multi-organ disorder, not just limited to the liver [11]. HCV can be acute or chronic. An acute HCV is a short-term infection of the virus that occurs during the first six months after exposure to HCV and presence of HCV RNA in the serum [12]. An acute HCV infection becomes chronic disease if unable to clear the virus from their system within six months of infection without therapeutic intervention; approximately 70% - 80% of those with an acute infection develop chronic HCV [13]. India has reported a prevalence of 3.02% in Andhra Pradesh [14] and 1.6% in Lucknow [15] and Agra recorded a seroprevalence rate 1% [16]. Despite this high prevalence, prior research has shown that many younger in 30 are unaware of their status [17]. HCVinfected persons have been estimated to incur twice the annual health care expenses and require hospitalization at three times the rate of HCV-uninfected individuals [18]. Current status of HCV in health care was lacking which gave a burden to us find a current prevalence of HCV in south Indian patients with liver diseases.
Materials and Methods
Study population
Total of 69,353 patients with liver diseases were screened for HCV in Hepatology department of Rajiv Gandhi Government General public health Hospital. Male patients were 34,281 and female were 35,072.
Ethical clearance
Study was conducted in accordance with ethics research committee and ethical clearance was obtained from ethics research committee of institution. Patient’s consent forms were received from all the patients for conducting present study.
Methodology
Patient’s age, weight, clinical, socio-demographic, anthropometric, and biological data were collected and recorded.
Sample collection and analysis
Patients blood samples were collected from 69,353 patients with liver diseases in the hepatology department and clotted blood samples were spun in a centrifuge at 2500 rpm for 20 minutes to separate the serum which was used for the analysis. Tests were included to rule out various co-morbid conditions of patients with liver diseases. LFT and RFT tests were performed in EM-360. Creatinine, Bilirubin level, Albumin and Prothrombin time were also done for the study subjects and recorded in the standard data collection sheets. Blood sugar level was also estimated for the prevalence of Diabetes mellitus among the HCV reactive patients. Initially, all the serum samples were screened for HCV using rapid test device (Reliable Pro-detect Biomedical Ltd, India) which detects based on the principle of lateral flow chromatographic immunoassay for the qualitative detection of IgM of HCV in human serum. Reactive specimen was confirmed with RT-PCR [19].
Fibroscan
To detect liver stiffness especially transient hepatic elastography was used. 502 Touch model, Version 5. The scan was performed by experienced hepatologist and the results are commuted using software C1.2 and 1.3. The probes used are M+ probe which produces a central frequency of 3.5 MHz which measures stiffness to a depth of 25 to 65 mm. For obese individuals XL probe is used which produces a frequency of 2 MHz and can measure upto a depth of 75 mm. It can measure stiffen from 1.5 kPa to a maximum of 75 kPa (kiloPascal). A value of upto 6.5 kiloPascal (kPa) is normal. A value between 6.5 to 8 kPa correlates with Metavir F1/F2, 8 - 12.5 suggests F3 and value more than 12.5 suggest F4 (cirrhosis).
Fibrometer
Fibrometer is a panel of blood test intended as a surrogate marker of liver fibrosis, Cirrhosis and Necro - inflammatory activity. An algorithm calculates of Age, Platelets, Gender, Prothrombin index (INR), AST, Alpa 2 macroglobulin, Urea, Gamma glutamyl tramsferase to provide scores (from 0 to 1) and corresponding fibrosis stage and activity grade according to the Metavir Scoring System (F1 - F4). History of significant alcohol consumption of >30 g/day in men and >20 g/day in women were also recorded [20].
Statistical analysis
Data were expressed as percentages, student’s t-test done and p-values <0.05 were considered significant. Chi Square test and one way ANOVA were also done. Co-efficient of variation, Regression and correlation was calculated to find Statistical significance.
Results
A total of 69,353 patients with liver diseases were screened for HCV. Out of 69,353 patients, 916 (1.3%) patients were reactive for HCV which was overall current prevalence of HCV in our present study subjects. Among 69,353 patients male were 34,281 (48.4%) and females were 35,072 (50.6%). Out of 34,281 male patients 634 were serologically reactive and 180 were virologically reactive. Out of 35,072 female patients 282 were serologically reactive and 63 were virologically reactive. Statistical significantance was found in gender wise distribution between screened patients and serological reactive patients and number of screened patients and virological reactive patients (p-value-<0.000) (Table 1). To compared the serological and virological positive paitent with the study population, regression and correlation was calculated and the Comparison of intercepts: t=0.012 with 2 degrees of freedom; P=0.992A New findings of our present study were liner increase of HCV in patients who visited hepatology department. 22 patients were reactive for HCV in 2011, 54 in 2012, 122 were reactive in 2013, 309 in 2014 and 409 were reactive for HCV in 2015 (Figure 1). There was a double fold increase of prevalence of HCV between the years 2012 and 2013 and this may be due to invention of sensitive screening methods. One way ANOVA analysis also showed statistically significant (Table 2).
| HCV reactivity | Male | Female | Chi Square | P value |
|---|---|---|---|---|
| Serological reactive (n=916) | 634 | 282 | 268.998 | 0.000* |
| Virological reactive(n=243) | 180 | 63 | 110.749 | 0.000* |
*Statistically Significant
Table 1: Comparison of gender wise distribution between number of patients screened and serological reactive patients.
| Year of screening | Population screened | Population reactive for HCV | One way ANOVA |
|---|---|---|---|
| 2011 | 3460 | 22 | 0.012* |
| 2012 | 7392 | 54 | 0.012* |
| 2013 | 10950 | 122 | 0.012* |
| 2014 | 22315 | 309 | 0.012* |
| 2015 | 25236 | 409 | 0.012* |
*Statistically Significant
Table 2: One way ANOVA analysis to compare the liner prevalence of HCV based on year.
In our study, out of 916, HCV reactive patients, 49.7% were with No bad habits and 50.3% were with unhealthy habits of alcohol, smoking and IV drugs. 302, (33%) patients were with alcohol alone, 11, (1.2%) were with smoking alone. 10, (1.1%) patients were with only IV drugs, 113, (12.3%) alcohol+smoking, 10, (1.1%) alcohol+IV drugs and 15, (1.6%) alcohol+smoking+IV drugs (Figure 2). We tried to find the Co-morbid conditions of HCV. Multiple co-morbidities found in 2.2% of our patients. Chronic diseases were found in 41.8% of our patients and among 41.8%, 25.2% patients had CLD and 16.6% had CKD. 16.1% of our patients were with extra-hepatic co-morbidities and 39.9% were with absence of Co-morbid conditions (i.e., only HCV infection) (Figure 3). Elevation of biological markers and serum enzyme activity were also studied in our present study (S. protein-63.9%, ALT-50.6%, AST-50%, T. bilirubin-44.3%, Urea-36.1%, Creatinine-31.3%). In 35.1% male patients elevated SAP levels were found and in female 39.1%. Diabetic subjects were 20.9% among our HCV reactive study patients (Table 3). Detection of liver stiffness and indirect evidence of fibrosis by various methods was evaluated in our present study. Fibroscan detected liver stiffness well than fibrometer and ultrasound which detects indirect evidence of fibrosis when we compared fibroscan vs endoscopy and fibroscan vs ultrasound which was found statistically significant (p-value-<0.000) (Tables 4 and 5). Other new findings of our present study were 2.5% of our HCV reactive population was with Hepato Cellular Carcinoma (HCC). One fifth (1/5) of our HCV reactive patients were Diabetic subjects and 1/3 of HCV reactive patients were obese and among the obese individual’s men were 32.7% and women were 39.3%.
| Biological markers | Elevation level | Percentage |
|---|---|---|
| S.Protein | >6.5 g/ml | 63.9% |
| Alanine aminotransferase (ALT) | >40 Iu/ml | 50.6% |
| Aspartate aminotransferase (AST) | >40 Iu/ml | 50.3% |
| Bilirubin (Total) | >1 mg/dl | 44.3% |
| Urea | >35 mg/dl | 36.1% |
| Creatinine | >1.2 mg/dl | 31.3% |
| S.Alkaline phosphate (SAP) | M->119, F->141 U/l | M-35.5%, F-39.1% |
| Blood Glucose | >140 mg/ml | 20.9% |
Table 3: Elevated biological markers in HCV reactive study population.
| Methods of detecting stiffness and indirect evidence of fibrosis | P value | ||
|---|---|---|---|
| Fibroscan | vs | Endoscopy | |
| 86 | 6 | ||
| Fibroscan | vs | Ultrasound | <0.000* |
| 86 | 9 | ||
*Statistically Significant
Table 4: Methods of detecting liver stiffness and indirect evidence of fibrosis among the study population.
| Year of screening | Population screened | Population reactive for HCV | Crude incidence rate |
|---|---|---|---|
| 2011 | 3460 | 22 | 6.358 |
| 2012 | 7392 | 54 | 7.325 |
| 2013 | 10950 | 122 | 11.141 |
| 2014 | 22315 | 309 | 13.847 |
Table 5: Crude incidence rate analysis to compare the liner prevalence of HCV based on year.
Discussion
Our current prevalence study findings were serological and virological prevalence among the HCV population. Higher numbers of females were screened but higher numbers of HCV reactive patients were male. Daniel et al. [21] showed that women had lower liver enzyme levels and HCV RNA compared with men which were compatible with our study. One way ANOVA and Chi Square showed that in our current study linear prevalence of HCV were found among the population.
Linear Increase of HCV by year can be by many factors, one factor can be alcohol, smoking and IV drug use which also pays a role in higher mortality among the HCV patients. Our present study shows that alcohol and smoking were in higher number in HCV patients with liver complication. Adding on the above findings Novo et al. [22] showed that combined effects of HCV and alcohol will potentially increases many mechanisms of liver damage. Liver diseases with HCV worsen not only by alcohol and smoking but co-morbidites of these patients increase the mortality. Negro et al. [23] found that a significant portion of the morbidity and mortality associated with HCV is a consequence of numerous HCV-associated co-morbidities. In our present study Among the co-morbidities of HCV patients CLD and CKD were in higher percentages. Butt et al. [24] added in his study that anti- HCV status was associated with low glomerular filtration rate. Our HCV patients with CKD need a special care. Extra-hepatic comorbidities also found in our study patients with considerable percentages. Cacoub et al. [25] found that HCV chronic infection should be analyzed as a systemic disease in which extra-hepatic consequences increase the weight of its pathological burden.
To find out the real burden of HCV in liver diseases patients a primary screening of liver enzymes will be essential and in our present study of HCV patients among the liver diseases showed elevated liver enzymes. Sette et al. [26] found that serum aminotransferase levels were lower in the patients with chronic kidney disease on hemodialysis (with or without viral hepatitis) than in the patients with normal renal function, this reduction has a multi-factorial origin. Along with biological liver enzymes markers other non-invasive markers like fibroscan also may help our HCV patients with liver diseases. In our study we found that fibroscan were the best way to find the liver stiffness. We calculated fibroscan with the cutoff value of 11 kpa. Barone et al. [27] calculated the risk to develop endothelial dysfunction and the cutoff value of >11.5 kpa.
As our study was the prevalence of HCV among liver diseases patients we studied other diseases and disorders and found a considerable percentage of HCC patients also were found in our study population. McMahon et al. [28] found that early identification, early identification of recurrence and better phenotyping of tumor in HCC patients will help them. Diabetes also was also a disorder found in the 1/5 population of our study subjects. Serfaty et al. [29] found that HCV-related type 2 diabetes mellitus may arise from a complex interaction between steatosis and inflammatory processes. 1/3 of our patients were also obese and Slama et al. [30] found that Obesity are strong risk factors and Increased waist circumference (excess of abdominal body fat) in obese patients is deleterious.
In conclusion, our study showed the liner prevalence of HCV by year. Serological and virological HCV population based on gender wise distribution showed that higher number of patients were male. Higher numbers of HCV patients were with bad habits in our study population. Our population showed co-morbid conditions, CLD were found in high number. Diabetic and obese subjects were in a considerable percentage in our study of HCV patients with liver diseases. Elevation of serum liver enzymes and fibroscan is the best non-invasive method for detecting liver stiffness in our study.
References
- GatselisNK,Dalekos GN (2011) Hepatobiliary and pancreatic: primary hepatic lymphoma. Journal of Gastroenterology and Hepatology 26: 210.
- MaYJ, Chen EQ, Wang J, Tang H (2010) Progress in research of primary hepatic lymphoma. World Chinese Journal of Digestology 18: 2790-2793.
- Gao J,Liu J, Hou L (2012) Report of one case of primary hepatic T cell lymphoma. Chinese Medical Imaging Technology 28: 1952.
- Li Z, He J, Zhu Y, Wu X (2014) CT manifestation of primary liver lymphoma. Medical Imaging Technology 24: 1762-1764.
- Luxon B (2011) Bone disorders in chronic liver diseases. CurrGastroenterol Rep 13: 40-48.
- Fede G, D’Amico G, Arvaniti V, Tsochatzis E, Germani G, et al. (2012) Renal failure and cirrhosis: a systematic review of mortality and prognosis. J Hepatol56: 810-818.
- Rahman S, Mallett SV (2015) Cirrhotic cardiomyopathy: Implications for the perioperative management of liver transplant patients. World J Hepatol7: 507-520.
- Ciccone MM, Principi M, Ierardi E, Di Leo A, Ricci G, et al. (2015)Inflammatory bowel disease, liver diseases and endothelial function: is there a linkage?. J Cardiovasc Med 16: 11-21.
- Nwokedi EE, Ilyasu Z, Emokpae MA, Dutse AI, Taura AA (2006) Hepatitis C virus infection among Teaching Hospital patients in Kano, Nigeria: A retrospective study. Ann Afr Med5: 185-187.
- Blachier M, Leleu H, Peck-Radosavljevic M, Valla DC, Roudot-Thoraval F (2013) The burden of liver disease in Europe: a review of available epidemiological data. J Hepatol 58: 593-608.
- A. Meillier, McGee J, Kartan S, Baskin S (2014) A case of multiple extrahepatic manifestations in a patient with untreated, chronic hepatitis C virus infection. International Journal of Infectious Diseases19: 93-94.
- AmanW, MousaS, ShihaG (2012) Current status and future directions in the management of chronic hepatitis C. Virology Journal 9: 57-59.
- FilipowiczSM (2010) Interferon therapy of hepatitis C: molecular insights into success and failure. Swiss Med Wkly 140: 3-11.
- Ponamgi SP, Rahamathulla S, Kumar YN, Chandra M, Lakshmi N, et al. (2009) Prevalence of hepatitis C virus (HCV) coinfection in HIV infected individuals in south India and characterization of HCV genotypes. Indian J Med Microbiol27: 12-16.
- Tripathi AK, Khanna M, Gupta N, Chandra M (2007) Low prevalence of hepatitis B virus and hepatitis C virus co-infection in patients with human immunodeficiency virus in Northern India. J Assoc Physicians India 55: 429-431.
- Hussain T, Kulshreshtha KK, Sinha S, Yadav VS, Katoch VM (2006) HIV, HBV, HCV, and syphilis co-infections among patients attending the STD clinics of district hospitals in Northern India. Int J Infect Dis 10: 358-363.
- Korthuis PT, Feaster DJ, Gomez ZL, Das M, Tross S, et al. (2012) Injection behaviors among injection drug users in treatment: the role of hepatitis C awareness.Addict Behav37: 552-555.
- Davis KL, Mitra D, Medjedovic J, Beam C, Rustgi V(2011) Direct economic burden of chronic hepatitis C virus in a United States managed care population. J ClinGastroenterol45: e17-e24.
- Arash G,Czeslaw W,Chao Lin,Stephen M, Feinstone et al. (1993) Expression and Identification of Hepatitis C Virus Polyprotein Cleavage Products. Journal of Virology 67: 1385-1395.
- LaBrecque DR, Abbas Z, Anania F, Ferenci P, Khan AG, et al. (2014) World Gastroenterology Organisation global guidelines: Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. J ClinGastroenterol48: 467-473.
- Corsi DJ, Karges W, Thavorn K, Crawley AM, Cooper CL (2016) Influence of female sex on hepatitis C virus infection progression and treatment outcomes. European Journal of Gastroenterology & Hepatology28: 405-411.
- Novo-Veleiro I, Alvela-Suárez L, Chamorro AJ, González-Sarmiento R, Laso FJ, et al. (2016) Alcoholic liver disease and hepatitis C virus infection. World journal of gastroenterology22: 1411.
- Negro F (2014) Facts and fictions of HCV and comorbidities: Steatosis, diabetes mellitus, and cardiovascular diseases. Journal of Hepatology 61: 69-78.
- Butt A, Wang X, Fried LF(2011) HCV infection and the incidence of CKD. Am J Kidney Dis 57: 396-402.
- CacoubP, Comarmond C, Domont F, Savey L, Desbois AC,et al. (2016)Extrahepatic manifestations of chronic hepatitis C virus infection. TherAdv Infect Dis 3: 3-14.
- Sette LH, Lopes EP (2014) Liver enzymes serum levels in patients with chronic kidney disease on hemodialysis: a comprehensive review. Clinics 69: 271-278.
- Barone M, Viggiani MT, Amoruso A, Schiraldi S, Zito A (2015)Endothelial dysfunction correlates with liver fibrosis in chronic HCV infection. Gastroenterology research and practice 2015.
- McMahon B, Block J, Block T, Cohen C, Evans AA, et al. (2016) Hepatitis-associated liver cancer: gaps and opportunities to improve care. J Natl Cancer Inst 108: 359.
- Serfaty L, Capeau J, Hepatitis C (2009) Hepatitis C, insulin resistance and diabetes: clinical and pathogenic data. Liver Int 29: 13-25.
- Slama L, Le Camus C, Serfaty L,Pialoux G, Capeau J,et al. (2009) Metabolic disorders and chronic viral disease: The case of HIV and HCV. Diabetes & Metabolism35: 1-11.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences