Laparoscopic Sphincter Saving Surgery for Node Positive Anorectal Melanoma
Vishwas D Pai, Manish Bhandare, Munita Bal and Avinash P Saklani
Vishwas D Pai1, Manish Bhandare1, Munita Bal2 and Avinash P Saklani1*
1Department of Surgical Oncology, Tata Memorial Centre, Mumbai, India
2Department of Pathology, Tata Memorial Centre, Mumbai, India
- *Corresponding Author:
- Avinash P. Saklani, MS, FRCS
Department of Surgical Oncology, Tata Memorial Centre, Ernest Borges Road, Mumbai 400012, Maharashtra, India.
Tel: +91-9969506719
E-mail: asaklani@hotmail.com
Received date: Deceember 07, 2015; Accepted date: January 09, 2016; Published date: January 15, 2016
Citation: Pai VD, Bhandare M, Bal M, et al. Laparoscopic Sphincter Saving Surgery for Node Positive Anorectal Melanoma. Colorec Cancer. 2016, 2:1. doi: 10.21767/2471-9943.100011
Abstract
Anorectal melanomas are very rare malignancies accounting for less than 1% of all the anorectal malignant tumors. There has been paradigm shift in the surgical management of these rare tumors over last decade from the more extensive abdominoperineal resection (APER) to the wide local excision (WLE). Non inferiority in survival, lower perioperative morbidity and better quality of life have been the factors contributing to faster adoption of WLE over APER. However local recurrence rate is significantly higher with WLE alone. The role of RT has not been well defined in anorectal melanoma. Hence there is a need for an alternative surgical procedure which may have lower recurrence rate while not compromising the quality of life of the patients. We are reporting laparoscopic intersphincteric resection for a case of anal melanoma which has all the advantages of the WLE and in addition, offers the advantage of wider margin as well as nodal clearance.
Introduction
Anorectal melanomas (ARM) are rare malignancies accounting for 0.4-0.6% of all melanoma cases and 1% of anorectal malignant tumors [1,2]. Surgery remains the gold standard treatment since melanoma are resistant to chemotherapy as well as radiotherapy. Conventionally two forms of surgical treatment are applicable for ARM–Abdominoperineal resection (APER) and wide local excision (WLE) [3]. Though WLE has been adopted as a safe alternative based on retrospective series, inabilities to dissect the mesorectal nodes as well as higher local recurrence are definite concerns with this procedure. We are describing a case of anorectal melanoma with involved mesorectal nodes treated by laparoscopic intersphincteric resection.
Methods
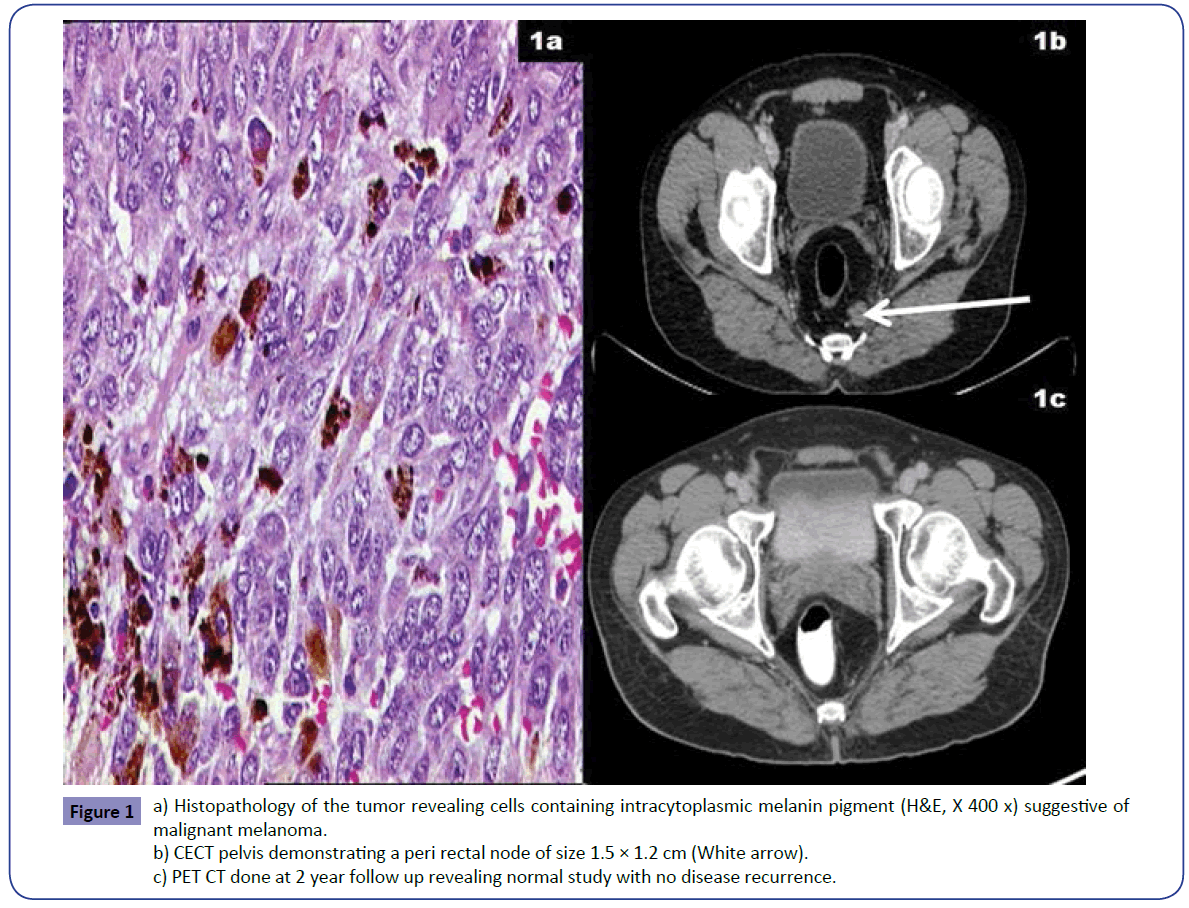
A 54 year old gentleman with history of perianal pain was found to have a solitary rectal polyp on rectal examination and underwent polypectomy at a peripheral hospital. Histopathological examination revealed malignant melanoma (Figure 1a) and hence he was referred to our centre. On presentation, there was an irregularity along the left lateral wall of rectum about 3 cm above the anal verge. Colonoscopy confirmed absence of any mucosal lesion. Contrast enhanced computed tomography (CECT) abdomen and pelvis revealed only distal rectal thickening and a peri rectal node of size 1.5 × 1.2 cm (Figure 1b). As the patient was very keen on conservation, laparoscopic intersphincteric resection was performed after explaining all the pros and cons of the procedure in detail. His intra and postoperative course was uneventful. Histopathological examination of the specimen revealed no residual lesion in rectum, with two of the nine nodes involved with perinodal extension. Patient was kept under observation. At 2 years follow up, patient is disease free with good bowel function (Figure 1c).
Figure 1: a) Histopathology of the tumor revealing cells containing intracytoplasmic melanin pigment (H&E, X 400 x) suggestive of malignant melanoma.
b) CECT pelvis demonstrating a peri rectal node of size 1.5 × 1.2 cm (White arrow).
c) PET CT done at 2 year follow up revealing normal study with no disease recurrence.
Discussion
ARM is an aggressive malignancy with dismal prognosis with an estimated five-year overall survival of 20–22% and a diseasefree survival of 16–17% [4,5]. Surgeryremains the mainstay of treatment since ARM does not respond to other forms of therapy. Surgical management of ARM is highly debated. There are generally two standard surgical approaches APER or WLE. Conventionally APER was the preferred surgical approach for these rare malignancies [3]. However a couple of studies in the late 1990s demonstrated equivalent survival rate and significantly lower perioperative morbidity with WLE in comparison with APER [3,6]. In addition lymph node status has not been linked to survival in ARM unlike in cutaneous melanoma. It has been observed that in majority of the patients of ARM, mortality occurs due to the development of distant metastasis. Also APER leads to permanent stoma and hence significantly poor quality of life. All these factors lead to the suggestion that WLE should be the initial procedure for ARM [7].
However Nilsson et al found that completeness of resection was the single most important prognostic factor with 5-year overall survival of 19% for patients with an R0 resection as opposed to 6% for patients with R+ resections [8]. They also noted that, APER was significantly more likely to achieve an R0 resection (76%) compared to a WLE (26%). Even the studies that showed non inferior survival with WLE did find significantly higher local recurrence with WLE compared to APER [3,7]. Local recurrence rates as high as 65% have been documented in literature with WLE alone [9]. It has been observed that lymph nodes are involved in 60% of patients of ARM at presentation [10]. Danielle et al observed that patients with ARM who underwent WLE more frequently recurred in the mesorectal nodes compared to those who underwent WLE [11]. Though sentinel lymph node mapping has been reported in short case series, none of these are large enough to draw firm conclusions on the effect of such mapping on recurrence or survival [12].
In view of these findings, laparoscopic intersphincteric resection may be a good alternative in these cases. Like APER, it can result in wider margins, comprehensive lymph node clearance, an improved R0 resection and hence probably lower local recurrence rate. Like WLE, it can avoid a permanent stoma, lower perioperative morbidity and hence superior quality of life. We have previously published the steps of the procedure and the short term results in cases of rectal adenocarcinoma and have found acceptable perioperative morbidity with laparoscopic intersphincteric resection [13].
Conclusion
Laparoscopic intersphincteric resection may provide a viable alternative to APER as well as WLE in the management of ARM. Larger studies adopting intersphincteric resection for cases of anorectal melanoma are needed to draw firm conclusions.
References
- Goldman S, Glimelius B, Pahlman L (1990)Anorectal malignant melanoma in Sweden. Report of 49 patients. Dis Colon Rectum 33:874-877.
- Weinstock MA (1993) Epidemiology and prognosis of anorectal melanoma. Gastroenterology104: 174-178.
- Brady MS, Kavolius JP, Quan SH (1995)Anorectal melanoma. A 64-year experience at Memorial Sloan-Kettering Cancer Center. Dis Colon Rectum 38:146-151.
- Meguerditchian AN, Meterissian SH, Dunn KB (2011)Anorectal melanoma: diagnosis and treatment. Dis Colon Rectum 54:638-644.
- Yeh JJ, Weiser MR, Shia J, Hwu WJ (2005) Response of stage IV anal mucosal melanoma to chemotherapy. Lancet Oncol 6:438-449.
- Iddings DM, Fleisig AJ, Chen SL, Faries MB, Morton DL (2010) Practice patterns and outcomes for anorectal melanoma in the USA, reviewing three decades of treatment: is more extensive surgical resection beneficial in all patients? Ann SurgOncol 17:40-44.
- Zhou H, Zhou Z, Zhang H, Bi J, Zhao P (2010) Wide local excision could be considered as the initial treatment of primary anorectalmalignant melanoma. Chin Med J 123:585-588.
- Nilsson PJ, Ragnarsson-Olding BK (2010) Importance of clear resection margins in anorectal malignant melanoma. Br J Surg 97:98-103.
- Che X, Zhao D-B, Wu Y-K, Wang C-F, Cai JQ, et al. (2011) Anorectal malignant melanomas: retrospective experience with surgical management. World J Gastroenterol 17:534-539.
- Chang AE, Karnell LH, Menck HR (1998) The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer 83:1664-1678.
- Bello DM, Smyth E, Perez D, Khan S, Temple LK,et al. (2013) Anal versus rectal melanoma: does site of origin predict outcome? Dis Colon Rectum 56:150-157.
- Mariolis-Sapsakos T, Malamitsi J, Yakoumakis E, Orfanos F (2008)Is sentinel node mapping useful in anorectal melanoma? Hell J Nucl Med11:39-42.
- Pai VD, Desouza A, De Menezes JL, Saklani AP (2015) Laparoscopic intersphincteric resection and hand-sewn coloanal anastomosis: a natural orifice specimen extraction technique. J LaparoendoscAdvSurg Tech A25:396-400.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences