CT or MRI Which is better for Rectal Cancer Imaging?
Rajul Rastogi, Meena GL, Yuktika Gupta, Pragya Sinha, Pankaj Kumar Das, Mohini Chaudhary and Vijai Pratap
DOI10.21767/2471-9943.100028
Rajul Rastogi1*, Meena GL2, Yuktika Gupta1, Pragya Sinha1,Pankaj Kumar Das1, Mohini Chaudhary1 and Vijai Pratap1
1Teerthanker Mahaveer Medical College& Research Centre, Moradabad, Uttar Pradesh, India
2S.P. Medical College and PBM Hospital, Bikaner, Rajasthan, India
- *Corresponding Author:
- Rajul Rastogi
Department of Radio Diagnosis, Teerthanker Mahaveer Medical College & Research Center, Moradabad, Uttar Pradesh, India.
Tel: 919319942162
E-mail: eesharastogi@gmail.com
Received date: September 01, 2016; Accepted date: September 19, 2016; Published date: September 26, 2016
Citation: Rastogi R, Meena GL, Gupta Y, et al. CT or MRI – Which is better for Rectal Cancer Imaging?. Colorec Cancer 2016, 2:3.
Abstract
Colorectal cancer is one of the common causes of cancer-related mortality with rectal cancer representing a significant proportion. Cross-sectional imaging techniques especially computed tomography (CT) and magnetic resonance imaging (MRI) play an important role in preoperative staging of rectal cancer. There has always been a debate about the single best imaging modality for staging of rectal cancer in order to achieve the best surgical outcome. Hence, this article focuses on the comparative role of CT & MRI in staging of rectal cancers.
Keywords
Colorectal; Rectal; Cancer; Computed tomography; Magnetic resonance imaging
Introduction
Colorectal cancer is second most common malignancy worldwide representing fourth commonest cause of cancer-related mortality [1]. More than a third of these occur in rectum near the anal verge [1,2]. Cross-sectional imaging modalities like computed tomography (CT) and magnetic resonance imaging (MRI) is usually the first tool for evaluation of suspected cases of rectal cancer that not only help in detection but also in local staging as well as in delineating the distant spread of cancer. With the advent of preoperative neoadjuvant chemoradiation therapy and increasing en-bloc resection of mesorectum to reduce postsurgical recurrence, local staging has assumed great significance [3]. Hence, this review article primarily focuses on the role of CT and MRI in local staging for preoperative evaluation of rectal cancer.
Discussion
The outcome of rectal cancer as with any other cancer depends largely on local and distant staging or in short, the TNM staging system. T1 tumor extends up to submucosa while T2 tumor reaches up to muscularis propria. T3 tumor extends beyond the muscularis propria in to the mesorectum while T4 tumors involve visceral peritoneum, adjacent structures (like prostate, seminal vesicles, uterus, vagina, lateral pelvic walls & sacrum) or levator ani muscle with or without anal sphincters. T3 tumor is further divided in to T3a & T3b based on extension of tumor beyond muscularis propria in to mesorectum by <5 mm and >5 mm respectively.
Both T1 & T2 tumors are treated almost similarly in most cases while T3 tumors show reduced risk of recurrence when treated preoperatively with chemotherapy and / or radiation therapy [3,4]. T3b tumor is associated with poorer 5-year survival rates than T3a tumor [5]. Besides the T-stage, the proximity of tumor to mesorectal fascia also affects the prognosis in cases of rectal cancer as tumor within 1 mm of this fascia, also known as circumferential resection margin (CRM) is associated with significantly increased risk of recurrence [6]. T4 tumor with involvement of sphincteric complex may necessitate abdominoperineal resection with en bloc resection of sphincter complex.
N-stage denotes the involvement of locoregional nodes in the mesorectum & pelvis by rectal cancer. The short-axis criterion of 5 mm diameter of mesorectal node gives a sensitivity of less than 70% but a specificity of nearly 80% of harbouring metastases [4]. Presence of nodes adjacent to mesorectal fascia may necessitate wider surgical margin while presence of nodes outside the mesorectum may need wider radiation field in addition to wider surgical margin [2,3]. Involvement of obturator, external iliac or retroperitoneal nodes corresponds to M1 stage.
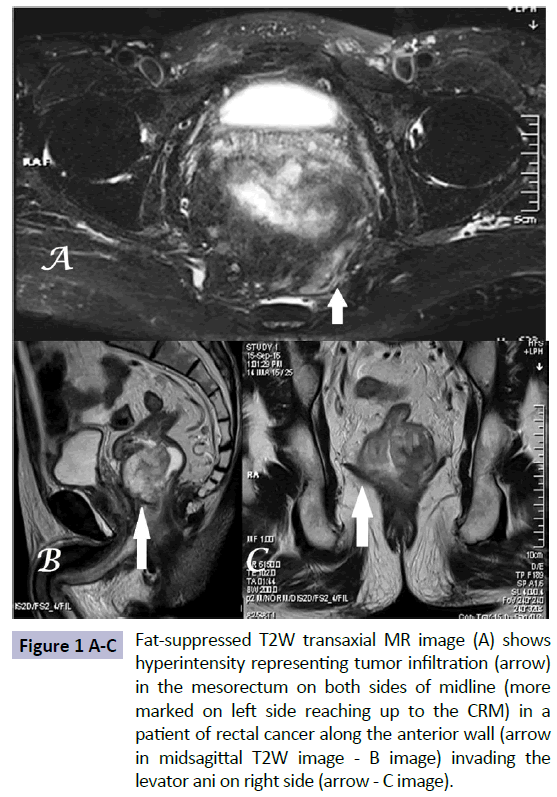
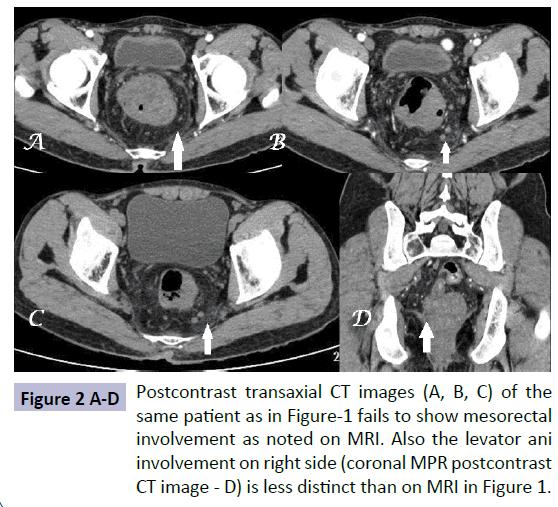
High-resolution MRI of pelvis with distension of rectum by positive contrast agent is an investigation of choice for local staging of rectal cancer due to its superior soft tissue contrast resolution. MRI is definitely superior to CT in local staging except in T1 & T2 stage where both have comparable accuracies [7] (Figures 1 and 2). Though T2W images in axial plane play a key role yet sagittal images are equally important in infiltrative tumors and tortuous rectum. Coronal images are especially useful in detecting levator ani & sphincteric complex involvement. Rectal cancer as well as the involved node appears hyperintense on DW images with slight hypointensity on ADC maps though it is not specific for metastatic nodes. Involvement of mesorectum and CRM is very well predicted by MRI with specificity of up to 95% [4].
Figure 1 A-C Fat-suppressed T2W transaxial MR image (A) shows hyperintensity representing tumor infiltration (arrow) in the mesorectum on both sides of midline (more marked on left side reaching up to the CRM) in a patient of rectal cancer along the anterior wall (arrow in midsagittal T2W image - B image) invading the levator ani on right side (arrow - C image).
For nodal involvement the size criterion of 5 mm in mesorectum and 10 mm in regional & distant nodes does not offer any major advantage of MRI over CT but more accurate detection of ancillary findings like irregular node, abnormal signal or pattern of enhancement of node make MRI slightly superior to CT (Figures 2 and 3).
For distant spread, MRI has limited role in detecting pulmonary parenchymal metastases less than 10 mm in diameter where CT scores over MRI. Role of MRI in detecting distant spread in cases of rectal cancer is reserved as a problem solving tool in sub centimeter hepatic lesions where the diagnosis of cyst / hemangioma or metastatic lesion is in question. In such cases, MRI is superior to CT as metastasis is hypointense on T1W and hyperintense on T2W (though less hyperintense than cyst / hemangioma) & DW images showing peripheral contrast enhancement [8,9].
Conclusion
MRI is superior to CT in local staging of rectal cancer helping the surgeon in preoperative planning to achieve negative surgical margins. For nodal staging and distant spread, CT & MRI show similar performance except in small pulmonary metastases where CT is superior to MRI and small hepatic metastases where MRI is excellent.
References
- Samee A, Selvasekar CR (2011) Current trends in staging rectal cancer. World J Gastroenterol 17: 828-834.
- Dewhurst CE, Mortele KJ (2013) Magnetic resonance imaging of rectal cancer. Radiol Clin North 51: 121-131.
- Kaur H, Choi H, You YN (2012) MR imaging for preoperative evaluation of primary rectal cancer: practical considerations. Radiographics 32: 389-409.
- Raman SP, Chen Y, Fishman EK (2015) Evolution of imaging in rectal cancer: multimodality imaging with MDCT, MRI, and PET. J Gastrointest Oncol 6: 172-184.
- Merkel S, Mansmann U, Siassi M (2001) The prognostic inhomogeneity in pT3 rectal carcinomas. Int J Colorectal Dis 16: 298-304.
- Samdani T, Garcia-Aguilar J (2014) Imaging in rectal cancer: magnetic resonance imaging versus endorectal ultrasonography. Surg Oncol Clin N Am 23: 59-77.
- Jhaveri KS, Hosseini-Nik H (2015) MRI of rectal cancer: An overview and update on recent advances. AJR 205: W42-W55.
- Raman SP, Horton KM, Fishman EK (2012) Multimodality imaging of pancreatic cancer-computed tomography, magnetic resonance imaging, and positron emission tomography. Cancer J 18: 511-522.
- Berger-Kulemann V, Schima W, Baroud S (2012) Gadoxetic acid-enhanced 3.0 T MR imaging versus multidetector-row CT in the detection of colorectal metastases in fatty liver using intraoperative ultrasound and histopathology as a standard of reference. Eur J Surg Oncol 38: 670-676.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences