Defunctioning Stoma Reversal-does the Approach to Primary Surgery Influence the Post Operative Outcomes?
Rahul Bhamre, Vishwas D Pai, Avanish P Saklani
Rahul Bhamre, Vishwas D Pai and Avanish P Saklani*
Department of Surgical Oncology, Tata Memorial Centre, Mumbai 400012, India.
- *Corresponding Author:
- Dr. Avanish P Saklani
Associate Professor, Colorectal/Robotic Surgery, Department of surgical oncology, Tata memorial centre, Ernest Borges Marg, Parel, India-400012.
Tel: +91-9969506719
Fax: 905-569-4326
E-mail: asaklani@hotmail.com
Received date: November 23, 2015; Accepted date: December 14, 2015; Published date: December 21, 2015
Citation: Bhamre R, D Pai V, Saklani AP. Defunctioning Stoma Reversal-does the Approach to Primary Surgery Influence the Post Operative Outcomes?. Colorec Cancer 2015, 1:1. doi: 10.21767/2471-9943.100007
Abstract
Aim: to determine whether laparoscopic approach for primary surgery carries any advantage over open approach in terms of morbidity as well as other clinical outcomes.
Methods: This is a retrospective review of a prospectively maintained database including all the patients of rectal cancer who underwent stoma reversal at Tata memorial centre between 1st June 2013 and 31st May 2015. Variables compared between the two groups were demographic characteristics, prior abdominal surgeries, time interval from stoma creation to reversal, surgical technique employed, blood loss, delay in starting oral feeding, hospital stay, perioperative morbidity and mortality.
Results: Ninety eight patients who underwent stoma reversal were included in the study. They were divided into 2 groups–those in whom the primary surgery was open and those in whom the primary surgery was laparoscopic. The two groups were comparable in all baseline characteristics except for the type of proximal defunctioning stoma and technique of stoma reversal. Laparoscopic group had lesser blood loss and fewer postoperative complications although the difference didn’t reach statistical significance. Hospital stay and oral feeding were comparable between the two groups.
Conclusions: Although stoma reversal after laparoscopic surgery leads to lower blood loss and fewer complications, it doesn’t transform into shorter hospital stay. Larger prospective studies are needed to favour one approach over the other.
Keywords
Stoma reversal; Rectal cancer; Laparoscopic surgery
Introduction
Radical surgery with total or partial tumour-specific mesorectal excision remains the mainstay of treatment for rectal cancers. Advances in the management in the form of neoadjuvant chemoradiotherapy, staging with Magnetic resonance imaging [MRI], availability of staplers, acceptance of less extensive distal margins and improved perioperative care have lead to increase in the number of low and very low rectal cancers being treated by the surgeons around the world. Literature suggests that presence of a defunctioning stoma decreases the incidence as well as the severity of anastomotic leakage and is recommended in all patients undergoing low or ultralow anterior resections for rectal cancer [1,2]. As a result there has been significant increase in the number of defunctioning stoma in cases of rectal cancer surgeries.
Despite the advantages a defunctioning stoma offers, its creation binds the patient to a second surgical procedure. Stoma reversal procedure itself is associated with morbidity ranging from 3-40%, mortality ranging from 0-4% and re explorations upto 7% [3-5]. In addition it has been observed that stoma reversal may not be possible in 1/3rd to 2/3rd of the patients [2,6]. These results have lead many researchers around the world to question the need for defunctioning stoma in individual cases and avoid a defunctioning stoma whenever feasible.
Laparoscopic rectalcancer surgery has been proven as oncologically safe [7,8]. Compared with open surgery, laparoscopic surgery offers a number of benefits including earlier return of bowel function, less postoperative pain, shorter hospital stays, and a better quality of life. It has also been observed that median time to start adjuvant chemotherapy after the rectal cancer surgery is shorter in cases of laparoscopic surgeries compared to open surgeries [9]. The present study was undertaken to determine whether laparoscopic approach for primary surgerycarries any advantage over open approach in terms of morbidity as well as other clinical outcomes.
Materials and Methods
This is a retrospective review of a prospectively maintained database in the Division of Colorectal Surgery at the Tata Memorial Centre, Mumbai. Between June 1st 2013 and May 31st 2015, all patients undergoing stoma reversal were identified from this database. Those patients who had undergone defunctioning stoma creation during the primary surgery and stoma reversal after the completion of adjuvant therapy at our institute were included. Patients who had undergone defunctioning stoma creation for indications other than rectal cancer were excluded.
Stoma reversal was planned 6 weeks after completion of adjuvant therapy or primary surgery (For those who didn’t warrant adjuvant therapy). All these patients after completion of adjuvant therapy were subjected to X ray loopogram and completion colonoscopy (for those whose initial colonoscopy was incomplete) after detailed history and physical examination. Anal manometry was performed selectively whenever intersphincteric resection was performed or when anal sphincter tone was found to be reduced. Patients with normal X ray loopogram, normal basal and squeeze pressure on manometry and no other lesions on colonoscopy were planned for stoma reversal. When basal pressure was reduced or squeeze pressure was not sustained on anal manometry, pelvic floor exercises were advised for 3-6 weeks followed by reassessment for stoma reversal. Those with stricture at anastomotic site on X ray loopogram or physical examination were subjected to dilatation of the stricture followed by stoma reversal.
Stoma reversal was performed by a circumferential incision. The anastomotic technique employed was either a hand sewn endto- end anastomosis with or without resection, a hand sewn side-to-side with resection or a stapled anastomosis. In general, stapled anastomosis is preferred for ileostomy closure and hand sewn anastomosis is preferred for transverse colostomy closure. Closure of the abdominal wall was performed with Vicryl 2’0 and skin was closed with interrupted Ethilon 3’0 sutures. No intraabdominal or subcutaneous drainage was placed. Patients were started on oral feeds on the same evening of surgery and feeds were increased to full diet as tolerated by patients. Oral feeding was considered delayed if not started after 2nd post operative day or if feeding was interrupted later due to ileus or some other complications. Anastomotic leakage was defined clinically as features of intra-abdominal sepsis or radiologically as anastomotic leakage of contrast or any peri anastomotic collection requiring drainage. Exploratory laparotomy followed by reanastomosis and proximal defunctioning ileostomy was performed for those with hemodynamic instability.
Variables compared between the two groups were demographic characteristics, prior abdominal surgeries, time interval from stoma creation to reversal, surgical technique employed, blood loss, delay in starting oral feeding, hospital stay, perioperative morbidity and mortality. Statistical analysis was performed using SPSS 20.0 for Windows (SPSS, Inc, Chicago, IL). χ2 test or Fisher’s exact test, as appropriate were used to compare variables. The difference was considered significant if the P value was less than 0.05.
Results
Ninety eight patients were included in the study. Demographic characteristics are shown in Table 1. The two groups were comparable in all baseline characteristics except for the type of proximal defunctioning stoma and technique of stoma reversal. Patients in the laparoscopic group were older and had higher BMI compared to open group though the difference didn’t reach significance. Clinical parameters are compared in Table 2. Hospital stay and oral feeding were comparable between the two groups. Laparoscopic group had lesser blood loss and fewer postoperative complications although the difference didn’t reach statistical significance. Delay in stoma reversal was shorter in laparoscopic group than open group though the difference didn’t reach statistical significance (p value-0.389).
| Demographic characteristics | Open surgery (n = 78) | Laparoscopic surgery (n = 20) | p value |
|---|---|---|---|
| Age (In years) (Median) ( Range) | 48 (23-82) | 55 (25-84) | 0.082 |
| Sex (Male: Female) | 1.8:1 | 1.5:1 | 0.797 |
| BMI (Median) | 18.5 - 23 | >23 | 0.195 |
| Stoma type Transverse colostomy Ileostomy | 43 (55%) 35 (45%) | 3 (15%) 17 (85%) | 0.002 |
| Stoma creation Elective Emergency | 69 (88.5%) 9 (11.5%) | 19 (95%) 1 (5%) | 0.682 |
| Prior abdominal surgeries | 5 (6.4%) | 1 (5%) | 1.000 |
| NACTRT | 62 (79.5%) | 15 (75%) | 0.768 |
| Type of closure Hand sewn Stapled | 60 (77%) 18 (23%) | 6 (30%) 14 (70%) | 0.000 |
BMI- Body mass index; NACTRT- neoadjuvant chemoradiotherapy.
Table 1: Comparison of demographic characteristics between open and laparoscopic groups
| Clinical parameters | Open surgery (n = 78) | Laparoscopic surgery (n = 20) | p value |
|---|---|---|---|
| Blood loss (in ml) (Median) (Range) | 200 (20-1400) | 20 (50-750) | 0.084 |
| Hospital stay (in days) (Median) (Range) | 7 (3-54) | 7 (3 - 12) | 0.149 |
| Post operative morbidity | 16 (20.5%) | 2 (10%) | 0.351 |
| Delay in starting oral feeds | 13 (16.7%) | 3 (15%) | 1.000 |
| Median time interval between primary surgery and stoma reversal (in weeks) (Median) (Range) | 43 (11-195) | 25 (25- 68) | 0.389 |
Table 2: Comparison of perioperative outcomes between open and laparoscopic groups.
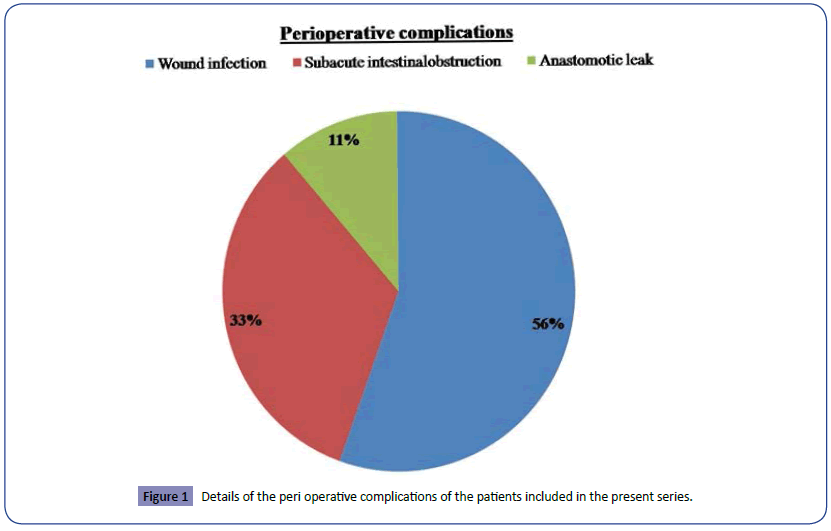
Perioperative morbidity was graded according to Clavin Dindo classification. Grade¾ complication developed in 18 patients (18.37%). Details of the perioperative morbidity are shown in Figure 1. Surgical site infection (SSI) was the most common complication. Ten patients in the open group and none in the laparoscopic group developed SSI. Among these 6 patients required prolonged antibiotics followed by secondary suturing whereas rest was managed conservatively. Sub-acute intestinal obstruction developed in 4 patients in the open group and 2 patients in the laparoscopic group. All 6 patients were managed conservatively and required extended hospital stay alone. Anastomotic dehiscence developed in two patients in the open group and none in the laparoscopic group. Both these patients required exploratory laparotomy with need for creation of new proximal diversion ileostomy.
Discussion
Laparoscopic surgery offers a number of advantages to the patients compared to open surgery in terms of lesser blood loss, early return of bowel functions, shorter hospital stay and fewer perioperative complications. Although stoma reversal is considered as a minor surgical procedure, it may be associated with significant post-operative morbidity. Present study was planned to compare perioperative outcomes between those who have undergone laparoscopic surgery and open surgery. Hypothesis is that laparoscopic surgery leads to fewer adhesions and makes the stoma reversal easier and leads to fewer complications.
There was a change in the unit protocol in 2013 with regards to defunctioning stoma creation in cases of rectal cancer from transverse colostomy to ileostomy. This corresponded with the inception a unit dedicated for colorectal onco surgery with significant increase in the number of minimally invasive surgical resections. This may explain higher incidence of ileostomy in the laparoscopic group compared to open group. In addition, although technique of stoma reversal is individualized, hand sewn end to end anastomosis without resection is preferred for transverse colostomy reversal whereas stapled end to end anastomosis with resection is preferred for ileostomy reversal. This explains the difference between the laparoscopic and open groups interms of techniques of stoma reversal in the present study.
Although the optimal time of stoma reversal after index surgery remains controversial, 6 weeks (8-12 weeks) is considered as the optimum time interval. This time period is essential to reduce the intra abdominaladhesion density, resolution of inflammation and optimum recovery of the patient from the index surgery [10]. A shorter time interval has been found to result in increased risk of complications whereas a longer time interval leads to inferior quality of life [11,12]. For those patients who require adjuvant therapy, stoma reversal is planned at the completion of the same [13]. In the present study the median time interval between primary surgery and stoma reversal was shorter for laparoscopic group than open group although it didn’t reach significance. Although this points towards early recovery from the primary surgery, this can’t be considered as the sole explanation for the observed findings.
Chow et al. in their systematic review of 6107 patients reported morbidity following stoma reversal of 17.3% and a mortality rate of 0.4% [10]. The most common complications in their analysis were intestinal obstruction followed by abdominal wall infection. In the present series there was no post-operative mortality and overall morbidity was 18.37% which in consistent with the systematic review. However, surgical site infection was the most common complication in the present series. Need for re surgery in the present series was lower compared to other series [14,15]. Factors leading to increase in the post-operative morbidity reported in literature include delay in the stoma reversal, adjuvant chemotherapy or radiotherapy and poor general health [16,17]. Limitation of the present study include retrospective nature of the study and hence the inherent selection bias, shorter sample size and variable approach followed for stoma reversal. However, to the best of our knowledge this is the first attempt to see the impact of approach for primary surgery on perioperative complication after stoma reversal.
Conclusion
Although stoma reversal after laparoscopic surgery leads to lower blood loss and fewer complications, it doesn’t transform into shorter hospital stay. Larger prospective studies are needed to favour one approach over the other.
References
- Wu SW, Ma CC, Yang Y (2014) Role of protective stoma in low anterior resection for rectal cancer: a meta-analysis. World J Gastroenterol20:18031–7.
- Jatal S, Pai V, Demenezes J, Desouza A, Saklani A (2015) Analysis of Risk Factors and Management of Anastomotic Leakage After Rectal Cancer Surgery: An Indian Series. Indian J SurgOncol 29: 1–7.
- DHaeninck A, Wolthuis AM, Penninckx FD, Hondt MD,HooreA(2011) Morbidity after closure of a defunctioning loop ileostomy.ActaChirBelg 111:136–141.
- Mengual-Ballester M, García-Marín JA, Pellicer-Franco E, Guillén-Paredes MP, García-García ML,et al.(2012) Protective ileostomy: complications and mortality associated with its closure. Rev EspEnferm Dig 104:350–354.
- Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, et al. (2009) The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis 24:711–723.
- Khan AA, Wheeler JMD, Cunningham C, George B, Kettlewell M, et al.(2008) The management and outcome of anastomotic leaks in colorectal surgery. Colorectal Dis 10:587–592.
- Kang SB, Park JW, Jeong SY, Nam BH, Choi HS,et al. (2010) Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvantchemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 11:637–645.
- van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, et al.(2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218.
- Sinukumar S, Mehta S, Ostwal V, Jatal S, Saklani A (2015) Impact of type of surgery (laparoscopic versus open) on the time to initiation of adjuvant chemotherapy in operable rectal cancers. Indian J Gastroenterol 34:310–313.
- Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E et al.(2009) The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis 24:711–723.
- Perez RO, Habr-Gama A, Seid VE, Proscurshim I, Sousa AHet al. (2006) Loop ileostomy morbidity: timing of closure matters. Dis Colon Rectum 49:1539–1545.
- El-Hussuna A, Lauritsen M, Bülow S (2012)Relatively high incidence of complications after loop ileostomy reversal. Dan Med J 59:A4517.
- Courtier R, Parés D, Silva CA, Gil MJ, Pascual Met al.(2012) Clinical results of loop ileostomy closures in rectal cancer surgical patients. Effect of chemotherapy in the waiting period. Cir Esp 88:308–313.
- Bakx R, Busch ORC, Bemelman WA, Veldink GJ, Slors JFM et al.(2004) Morbidity of temporary loop ileostomies. Dig Surg 21:277–281.
- Pérez Domínguez L, GarcíaMartínez MT, Cáceres Alvarado N, Toscano Novella A, HigueroGrosso AP, et al.(2014) Morbidity and mortality of temporary diverting ileostomies in rectal cancer surgery. Cir Esp 92:604–608.
- Thalheimer A, Bueter M, Kortuem M, Thiede A (2006) Meyer D. Morbidity of temporary loop ileostomy in patients with colorectal cancer. Dis Colon Rectum 49:1011–1017.
- Sharma A, Deeb AP, Rickles AS, Iannuzzi JC, Monson JRT, et al.(2013) Closure of defunctioning loop ileostomy is associated with considerable morbidity. Colorectal Dis 15:458–462.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences